Obtaining Medicare Coverage for Fleur-de-Lis Abdominoplasty Surgery
Medicare will only cover Fleur-de-Lis abdominoplasty if it is a medical necessity. There are two groups qualifying for MBS number: post-pregnancy cases involving muscle separation (Diastasis recti) and related symptoms and post-weight loss cases where the patient records a weight loss exceeding 5 BMI levels and maintains stable weight for at least 6 months.
Funding fleur de lis surgery can be costly and challenging. Therefore, most patients in Australia consider Medicare rebates to help cover the procedure’s cost. This is a viable option; however, Medicare has set strict criteria that patients must meet for eligibility.

Proof of medical necessity is the primary eligibility criteria for any surgical procedure. In addition, the procedure must be listed under the MBS Item Numbers. This can seem overwhelming at first glance, but this guide has everything you need.

Fleur-de-Lis Abdominoplasty Surgeries Qualifying for an MBS Item Number
Fleur-de-Lis Abdominoplasty provides more extensive tightening and fat removal than a traditional tummy tuck (abdominoplasty) procedure due to the vertical incision and additional excess skin involved. Abdominoplasty of any kind for cosmetic purposes is considered “cosmetic” and, therefore, not covered under Medicare. However, when a Fleur-de-Lis abdominoplasty procedure is performed for medical reasons. Medicare classifies eligible abdominoplasty procedures into two categories: post-pregnancy and post-weight loss.
Post-pregnancy
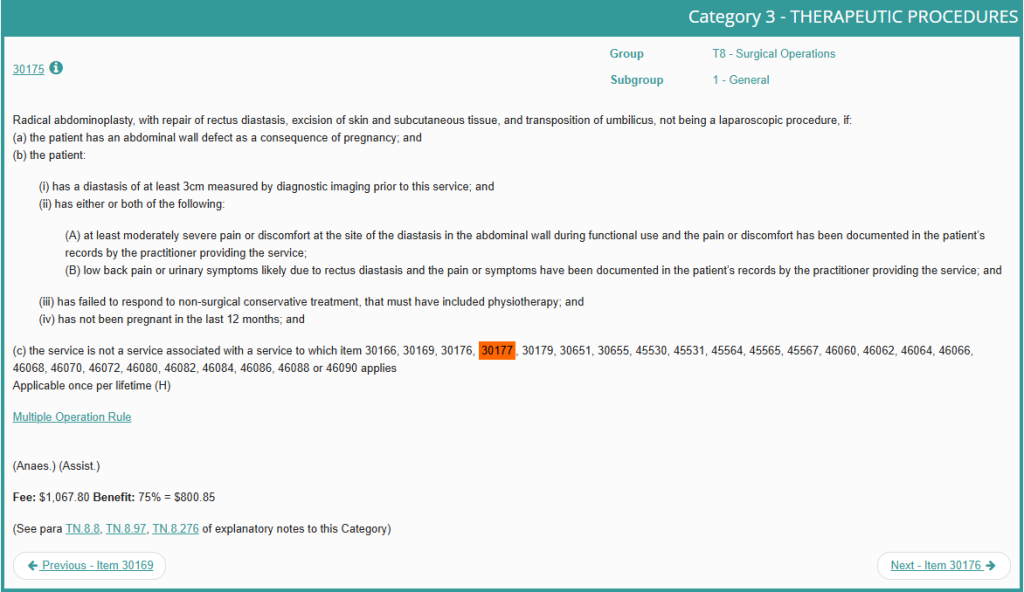
MBS item number 30175 for post pregnancy abdominoplasty | BCSC
Medicare offers rebates to post-partum patients undergoing fleur de lis surgery to cover separated abdominal muscles (diastasis recti) and redundant skin that causes medical conditions such as difficulty walking or performing tasks, discomfort, rashes, and infections.
Post-weight Loss
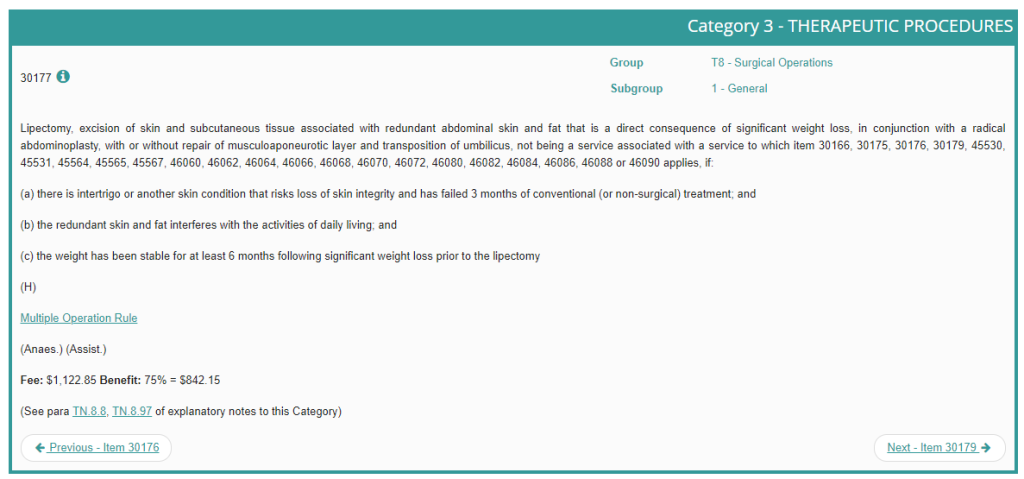
30177 MBS item number for abdominoplasty post weight loss | BCSC
Medicare covers patients undergoing FDL abdominoplasty (tummy tuck) to remove excess skin resulting from significant weight loss. Medicare describes significant weight loss as at least 5 BMI’s. In addition, the patient must have maintained a stable weight for a minimum of six months before body contouring surgery.
What is MBS (Medicare Benefits Schedule)?
Medicare is Australia’s universal health care medical insurance scheme. It is publicly funded and operated by Social Security. Medicare covers Australia’s citizens and permanent residents. Medicare covers essential standard procedures but has limited coverage for specialised surgical procedures, including abdominoplasty. MBS (Medicare Benefits Schedule) is a list of medical services that Medicare covers, including eligibility criteria and fees for each procedure. While all procedures have a unique MBS Item Number, only patients who qualify for an MBS Item Number are eligible to receive rebates.
Understanding Medicare and Private Health Insurance Coverage in Australia
Medicare helps provide financial relief to patients seeking healthcare. However, Medicare only covers procedures that are considered medically necessary, and does not offer coverage for cosmetic procedures. If the patient qualifies for a MBS Item Number, they can claim the procedure’s cost from their health fund.
However, Medicare only covers the fees listed on the Medicare Benefits Schedule (MSB), which might be lower than most specialist surgeons’ charges. Private health insurance, which also covers procedures with a MBS Item Number, offers more coverage than Medicare.
It’s important to note that despite having coverage, you must lay out the surgeon’s fee prior to undergoing the procedure. You can then claim the fees from the health fund and request a rebate. Medicare only covers a part of the total cost, leaving the patient to cover additional costs, such as the anaesthesia fee and hospital fees.
Patients with insurance can only claim rebates from their private health fund, not Medicare. After claiming from the private health fund, the fund will then claim the funds from Medicare. That is 75% of the scheduled fee. The hospital will bill the private health fund directly to cover any expenses incurred by the private health coverage.
What Medicare Will Cover in Australia
Below are the costs that Medicare covers for patients qualifying for rebates
- 100% of the costs to consult a GP (General Practitioner).
- 85% of the MBS scheduled out-of-hospital fees (follow-up appointments, consultation with specialists, pre-operative assessments, and post-operative care)
- 75% of the MBS scheduled in-hospital fees
What Medicare Will Not Cover in Australia
Medicare covers a portion of doctor’s fees but does not cover hospital fees, such as theatre and accommodation fees. In addition, most surgeons charge higher than Medicare’s scheduled fee, requiring patients to pay the extra fees out of pocket. This is because Medicare doesn’t review the scheduled fee regularly. This means Medicare rarely changes or adjusts the set fee amounts it will reimburse for different medical services. Therefore, the scheduled fees do not always keep pace with the actual cost for such services, which tend to rise over time due to inflation, advances in medical technology, and other factors.
One of the ways to stay ahead of this is by getting private health insurance.
What Private Health Insurance Covers in Australia?
Private health insurance offers higher coverage compared to Medicare. The costs covered by private health insurance include:
- A minimum of the full amount of the MBS scheduled fee for the surgeon
- A minimum of the total amount of the MBS scheduled fee for the anaesthetist
- A minimum of the total amount of the MBS scheduled fee for the surgeon’s assistant
- The total amount of the in-hospital fees
What Private Health Insurance Does Not Cover in Australia
Most private health insurance only covers medically necessary procedures covered by Medicare. Higher levels of private health insurance coverage, however, may cover cosmetic surgery in some instances. Patients should confirm their level of coverage with their insurance provider.

Cost Breakdown Examples
Example 1: Cost Breakdown for Patient With Insurance Undergoing Fleur de Lis Surgery for Medical Reasons and Qualifies for MBS Item Number
Patient presentation: Patient presents with weight loss of 40 kg, requires surgery to resolve medical issues, qualifies for an MBS item number, and has gold level health insurance.
Operation performed: FDL abdominoplasty
Surgery Time: Varies
Hospital Stay: 3-5 days
Hospital Fees: Covered by Health insurance
Surgeon’s Fees: $12,000 (rebate from health fund 1347.42 based on 120% of the MBS schedule fee)
Anaesthetist Fees: $3,600 (the rebate will depend on a number of factors including anaesthetic technique, around $400)
*Estimated Out-of-Pocket Cost: $13,852.58
Example 2: Cost Breakdown for Patient With No Insurance Undergoing Fleur de Lis surgery for Medical Reasons and Qualifies for MBS Item Number
Patient presentation: Patient presents with weight loss of 50 kg, requires surgery to resolve medical issues, qualifies for an MBS item number, but does not have private insurance.
Operation performed: FDL abdominoplasty
Surgery Time: Varies
Hospital Stay: 3-5 days
Hospital Fees: $14,000 for operation, $1,400 per day in hospital.
Surgeon’s Fee: $12,000 (Medicare rebate: $842.15 )
Anaesthetist Fee: $3,600 (Medicare rebate $200)
*Estimated Out-of-Pocket Cost: $31,357.85
Example 3: Cost Breakdown for Patient Undergoing Fleur de Lis surgery for Cosmetic Purposes with No Insurance or Medicare Coverage
Patient presentation: Patient presenting with loose skin on her abdomen does not qualify for either the post pregnancy or the post weight loss MBS item numbers because the surgery is considered cosmetic.
Operation performed: FDL abdominoplasty
Surgery Time: Varies
Hospital Stay: 3-5 days
Hospital: $14,000 for operation, plus $1,400 per day in hospital.
Total: $16,800, as operation is cosmetic the hospital will need to add 10% GST. Total cost 18,480 (government’s share: $1,680)
Surgeon: $12,000 need to add 10% GST Total: 13200 (government’s share: $1,320)
Anaesthetist: $3,600 need to add 10% GST Total $3960 (government’s share: $360)
*Estimated Out-of-Pocket Cost: $33,960 (Government’s Share: $3,360)
***Please note that these are simply estimates and the total cost will vary depending on a variety of factors including surgery time, days spent in the hospital, etc.

Known Gap Vs No-Gap
Medicare lists the scheduled fee for all the procedures with a MBS Item Number. However, most private clinics and hospitals specialising in these procedures charge more than what is stipulated by Medicare.
This leaves patients often having to pay an extra fee from their pockets. This is known as a “Gap.” This gives rise to two key terminologies used in private health insurance coverage, “No-Gap” and “Known-Gap.”
No-Gap
Under the no-gap type of coverage, the specialist surgeon accepts the amount the health fund or Medicare pays. This means that the patient doesn’t pay anything out of their pocket. However, the amount is lower compared to the actual cost of the procedure, as Medicare rarely revises their scheduled fees. If the specialist surgeon charges higher, the patient can take advantage of the “Known-Gap” from their private insurer.
Known-Gap
In the complex landscape of the Australian healthcare system, the term “known gap” frequently surfaces, yet its implications are not always fully understood by patients and healthcare providers alike. Essentially, the known gap pertains to the additional out-of-pocket expenses that patients may need to pay for medical services, over and above what is covered by Medicare and private health insurance. This arises when healthcare providers, such as doctors or specialists, charge fees that exceed the Medicare Benefits Schedule (MBS) rates.
Private health funds, in an effort to mitigate these costs for policyholders, administer known gap schemes that cap the additional fees specialists can charge. For example, the HCF Medicover scheme allows for an agreed-upon cap, typically up to $500 above the MBS rate. While this offers a level of financial predictability, it’s crucial to note that many specialist surgeons may opt out of these schemes due to payment structures that may not align with their service costs.
Due to the low level of the rebate provided, most specialist surgeons are not participating in these schemes.
Eligibility Requirements for Medicare Coverage of FDL Abdominoplasty
The first requirement for Medicare coverage for Fleur-de-Lis abdominoplasty is that the procedure be a medical necessity. It must be deemed essential for the body’s normal functioning and not simply be performed for cosmetic reasons. In addition, the patient should be undergoing Fleur-de-Lis procedure to remove excess tummy skin resulting from significant weight loss or to correct muscle separation resulting from pregnancy.
The first step to prove that Fleur-de-Lis abdominoplasty is medically necessary is visiting a GP (General Practitioner). The GP will assess your condition and medical history, among other factors, and document the symptoms to evidence the procedure is a medical necessity. The GP then refers you to a specialist surgeon.
Note that you cannot undergo a Fleur de Lis (Abdominoplasty) surgery without getting a referral from a GP. In addition, the GP’s referral is essential in claiming Medicare rebates. Note: Referrals are only valid for twelve months.
After getting a GP’s referral, the next step is to book a consultation with a qualified and experienced specialist surgeon. The specialist surgeon uses the GP’s information to determine if the condition is medically necessary. In addition, the specialist surgeon conducts a battery of tests to assess the patient’s eligibility to undergo Fleur-de-Lis tummy tuck (Abdominoplasty) surgery.
The patient must also demonstrate that they have tried non-surgical treatment remedies like a healthy diet and exercise for at least three months without success.
The surgeon then determines which MBS Item Number the patient qualifies for and gives the patient a quote of the procedure’s cost. This is why you should prepare for a consultation before planning the surgery to know what to expect, financially.
Medical Necessity Factors Ensuring Medicare Rebates
Let’s examine the factors proving medical necessity when applying for Medicare coverage.
Massive Weight Loss
The patient must have undergone massive weight loss prior to surgery. This weight loss can be the result of gastric bypass surgery or traditional methods. Medicare defines massive weight loss as at least 5 BMI, equivalent to fifteen kilograms. BMI (Body Mass Index) is the relationship between the body’s mass and weight. In addition, the patient must have maintained a stable weight for a minimum of six months after massive weight loss.
NOTE: For post-pregnancy women, weight is calculated by the woman’s weight before pregnancy. Therefore, you must have lost at least 5 BMI of your pre-pregnancy weight for your surgery to be deemed medically necessary for Medicare purposes.
Excess Skin Affecting the Body’s Normal Functioning
Fleur-de-Lis abdominoplasty helps remove excess skin on the lower and upper abdomen. Some patients may want to remove the excess skin for cosmetic reasons. However, for Medicare coverage, the excess skin must be affecting the patient’s ability to work and/or function in everyday life. Some situations include when the excess skin causes back pain, incontinence, rashes, or infections.
Skin rashes result from the excess skin rubbing against itself. This may also result in irritation, redness, and skin sores that can be painful. In addition, the folds on the excess skin may hold sweat and bacteria. They can be hard to clean, harbouring dirt and germs, causing infections and discomfort. A study on excess skin after massive weight loss notes, “[t]he number of patients experiencing discomfort from excess skin increased along with increased (amount of) ptosis (excess skin, but the correlation between ptosis size and QoL was low.”
This study examined the impact of excess skin after massive weight loss, focusing on physical discomfort and quality of life (QoL). It found that as the amount of excess skin (ptosis) increases, patients experience more physical discomfort, such as irritation. However, the study also revealed a low correlation between the size of ptosis and overall quality of life. This suggests that while larger amounts of excess skin cause more discomfort, they don’t necessarily lead to a significantly low QoL, indicating other factors may play a more prominent role in patients’ overall well-being.
Therefore, patients must also demonstrate that non-conventional treatment options to remove the excess skin have failed for a minimum of 3 months.
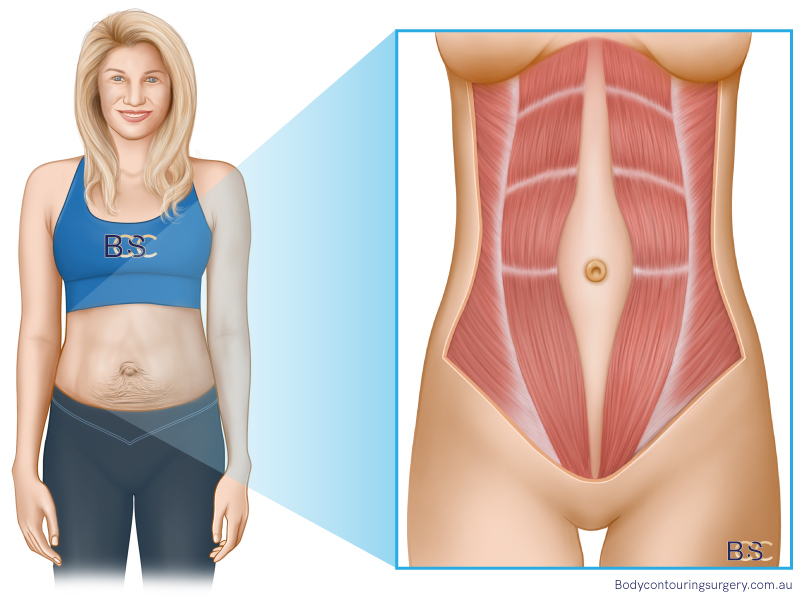
Separated Abdominal Muscles
Separated abdominal muscles (diastasis recti) are generally common in postpartum patients. The muscle separation may result in painful hernias and discomfort. In fact, according to a study published in Pubmed notes, “[a]fter pregnancy, some women experience severe rectus diastasis (RD), with body control dysfunction, midline hernia, or other quality-of-life impairment.”
Most specialist surgeons, including Dr. Beldholm, recommended Fleur-de-Lis abdominoplasty to treat hernias and reduce the risk of recurrence. The fleur-de-lis procedure often involves a vertical incision in addition to the horizontal incision, enabling the surgeon to remove excess skin and repair the muscle separation more comprehensively. The specialist surgeon uses testing like ultrasound to prove that the patient qualifies for an MBS item number.

MBS Item Numbers for Fleur-de-Lis Abdominoplasty Surgery
As noted earlier, qualifying for an MBS Item number for an abdominoplasty procedure involves strict criteria. The patient must also satisfy the significant weight loss or muscle separation (diastasis recti) criteria. Below are some MBS Item Numbers for all abdominoplasty surgeries, including FDL.
MBS Item Number 30166
MBS Item Number 30166 covers the excision of excess redundant abdominal skin and lipectomy, as a wedge excision, for functional problems following massive weight loss of at least 5 BMI (body mass index) points. The patient must have maintained a stable weight for a minimum period of 6 months before surgery.
Eligibility Requirements
- Must have undergone significant weight loss before the procedure. Medicare defines significant weight loss as equivalent to at least 5 body mass index (BMI) units.
- Maintained a stable weight for at least six months before the procedure, following significant weight loss
- The procedure is not intended to be a primary bariatric procedure for obesity correction.
- For pre-pregnancy significant weight loss that occurred before pregnancy, the weight directly associated with conception should not be included in the baseline weight calculation for measuring weight loss.

MBS Item Number 30175
MBS Item Number 30175 covers radical abdominoplasty procedures to repair rectus diastasis (separated abdominal muscles), skin and fatty tissue excision, and umbilicus (belly button) repositioning. The surgery should not be laparoscopic.
Eligibility Requirements
- The abdominal wall defect should be a result of pregnancy
- The patient presents a diastasis of the abdominal muscles of a minimum of 3 cm before the procedure, which should be proved by diagnostic imaging
- The patient experiences moderately severe discomfort or pain at the region of the diastasis during functional use, and the medical practitioner has adequately documented the symptoms
- The patient experiences urinary symptoms or low back pain likely resulting from diastasis rectus, and the medical practitioner has adequately documented the symptoms
- The patient has failed to react to non-surgical treatments, which included physiotherapy
- The patient has not been pregnant in the last twelve months
MBS Item Number 30177
MBS Items Number 30177 covers lipectomy, skin, and excess tissue excision due to redundant excess abdominal skin and fat that directly results from significant weight loss, including FDL abdominoplasty. The procedure includes a radical abdominoplasty, which may involve musculoaponeurotic layer repair and repositioning of the umbilicus (belly button).
Eligibility Requirements
- The patient has intertrigo or another skin condition that poses the risk of loss of skin integrity.
- Treatment of the redundant excess abdominal skin using non-surgical (or conventional) treatments has failed for at least 3 months.
- The redundant excess skin and fatty tissue affects the patient’s daily living.
- Maintained a stable weight for at least six months before the procedure, following significant weight loss.
Dr. Beldholm’s Final Thoughts

Many patients find it challenging to cover the cost of their Fleur-de-Lis surgery and can get assistance with private health insurance and seek rebates through Medicare. Medicare, however, imposes strict criteria for patient eligibility. Therefore, the procedure must be medically necessary and meet the set criteria. You can find everything in this article, or by booking a consultation in my office to learn more and discover if you’re eligible for Medicare coverage in Australia.
References
- Mitchell, R. T., & Rubin, J. P. (2014). The Fleur-De-Lis abdominoplasty. Clinics in plastic surgery, 41(4), 673–680.
- Friedman, T., O’Brien Coon, D., Michaels V, J., Purnell, C., Hur, S., Harris, D. N., & Rubin, J. P. (2010). Fleur-de-Lis abdominoplasty: a safe alternative to traditional abdominoplasty for the massive weight loss patient. Plastic and reconstructive surgery, 125(5), 1525–1535.
- Sperstad, J. B., Tennfjord, M. K., Hilde, G., Ellström-Engh, M., & Bø, K. (2016). Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. British journal of sports medicine, 50(17), 1092–1096.
- Tuominen, R., Peltoniemi, H., Jahkola, T., & Vironen, J. (2024). An Abdominoplasty Modification for Post Pregnancy Abdomen with Rectus Diastasis and Midline Hernia: The Technique and Results. Plastic and reconstructive surgery, 153(6), 1111e–1115e.
- Elander, A., Biörserud, C., & Fagevik Olsén, M. (2021). Excess skin after weight loss following bariatric surgery: focus on the abdomen. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery, 17(5), 986–993.
- Olsson, A., Kiwanuka, O., Wilhelmsson, S., Sandblom, G., & Stackelberg, O. (2021). Surgical repair of diastasis recti abdominis provides long-term improvement of abdominal core function and quality of life: a 3-year follow-up. BJS open, 5(5), zrab085.
- Michalska, A., Rokita, W., Wolder, D., Pogorzelska, J., & Kaczmarczyk, K. (2018). Diastasis recti abdominis — a review of treatment methods. Ginekologia Polska, 89(2), 97–101.
- https://www.health.gov.au/topics/medicare/about/what-medicare-covers
- https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=30166&qt=item&criteria=30166
- https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=30169&qt=item&criteria=30169
- https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=30175&qt=item&criteria=30175
- https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&qt=ItemID&q=30177
- https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=30179&qt=item&criteria=30179