Fleur-de-Lis Abdominoplasty Surgery Guide
Fleur-de-Lis is an abdominoplasty procedure involving a vertical and a horizontal incision intersecting at the groin region, forming an inverted T. The procedure helps remove loose skin in patients with major weight loss, which would be challenging to remove through standard abdominoplasty procedures.
This fleur de lis surgery guide helps elaborate further on Fleur-de-Lis abdominoplasty, the surgery process, recovery, pros and cons, suitability, and how to prepare for the procedure.
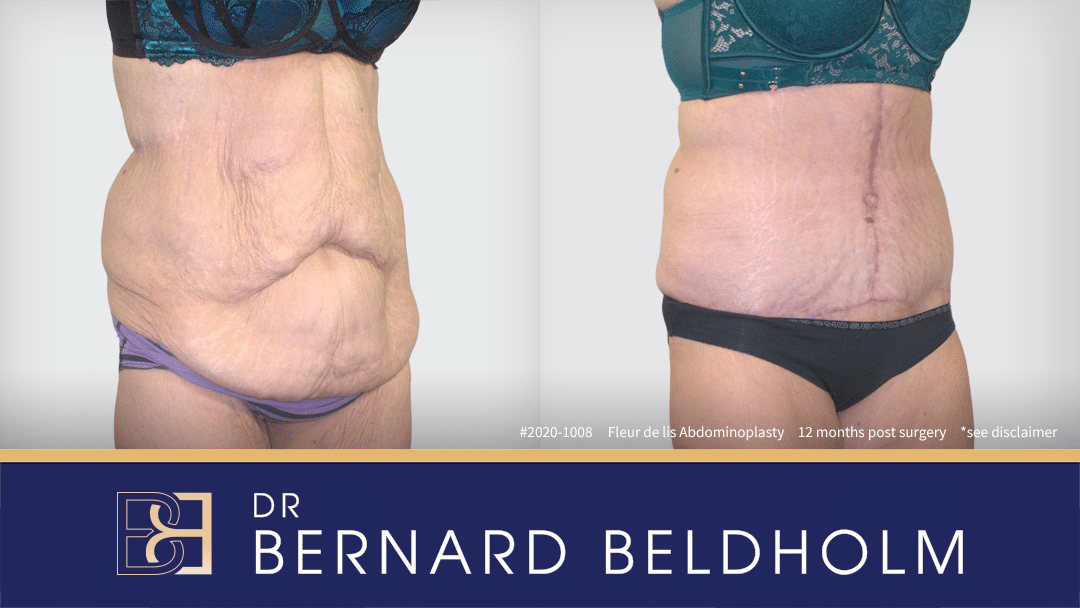
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
What is Fleur-de-Lis Abdominoplasty?
Fleur-de-Lis is a French term meaning “flower of the lily.” The name is derived from the inverted T procedure incision pattern, which looks like a partially closed three-petal flower. Fleur-de-Lis abdominoplasty removes excess skin and fat from the upper and lower abdomen and repairs abdominal muscles.
Fleur de lis | BCSC
Image: French water lilly illustration “fleur de lis”
The surgery involves a standard abdominoplasty incision (a horizontal hip-to-hip incision) and a vertical incision (running from the groyne area along the midline.) The length of the vertical incision depends on the amount of excess skin being removed in the midsection.

Preparing for Fleur-de-Lis Abdominoplasty
Before the procedure, you’ll meet with the surgeon for a consultation. Your surgeon will learn more about:
- Your general health.
- Your health history.
- Any previous surgeries.
- Any medications and supplements you currently take.
- Your goals and expectations for the fleur de lis procedure.
- Perform a physical exam.
Because smoking tobacco products can increase the risk of complications and delay healing, the surgeon will advise the patient to refrain from smoking for at least six weeks before and after the procedure.
The surgeon will also recommend that the patient eats a well-balanced diet both before and after the procedure as proper nutrition can help the body heal.
As part of the preoperative consultation, the surgeon may instruct you to stop taking certain blood-thinning medications and dietary supplements for a certain period before and after the surgery. This includes aspirin and nonsteroidal anti-inflammatories (NSAIDs).
Additional information will also be reviewed. In preparation for the surgery, the patient may need to:
- Ask someone to drive them to and from the procedure.
- Move frequently used items in the home so they are within arm’s reach.
- Choose loose and comfortable clothing.
- Use a hand-held shower head to bathe or use a bathroom chair for comfort.
- Consider installing a grab bar or removable raised toilet seat.
The surgeon will also answer any questions to offer comfort and ease pre-surgery anxiety.
Who is a Candidate for Fleur-de-Lis Abdominoplasty
Most Fleur-de-Lis abdominoplasty candidates are major post-weight loss patients with significant skin laxity in the upper abdomen. This significant weight loss could be the result of diet and exercise, bariatric or gastric bypass surgery, or post-pregnancy weight loss. In such cases, standard abdominoplasty may fail to adequately address the upper abdominal skin laxity.
Fleur-de-Lis abdominoplasty is also suitable for patients with pre-existing midline surgical scars in the upper abdomen, such as subcostal scars.
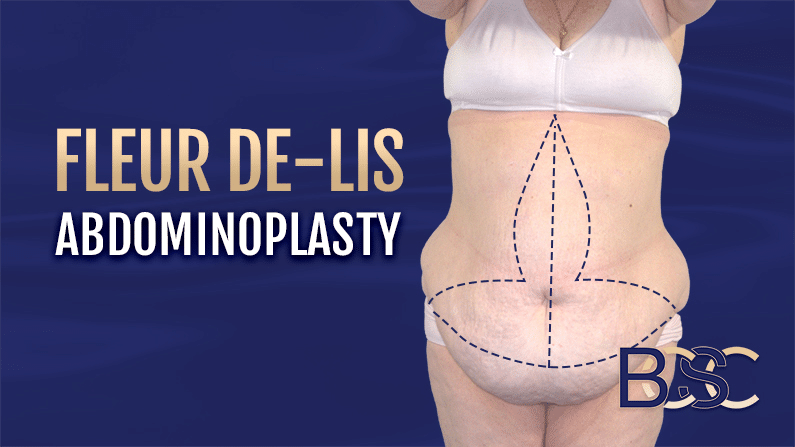
Fleur de lis abdominoplasty pattern | BCSC
Fleur-de-Lis Abdominoplasty vs. Mini Abdominoplasty
A mini abdominoplasty procedure is the least invasive abdominal body contouring procedure, addressing skin laxity only on the lower abdomen with no muscle separation repair. Fleur-de-Lis abdominoplasty, which is a more invasive surgery, addresses more abdominal regions and can also repair muscle separation.
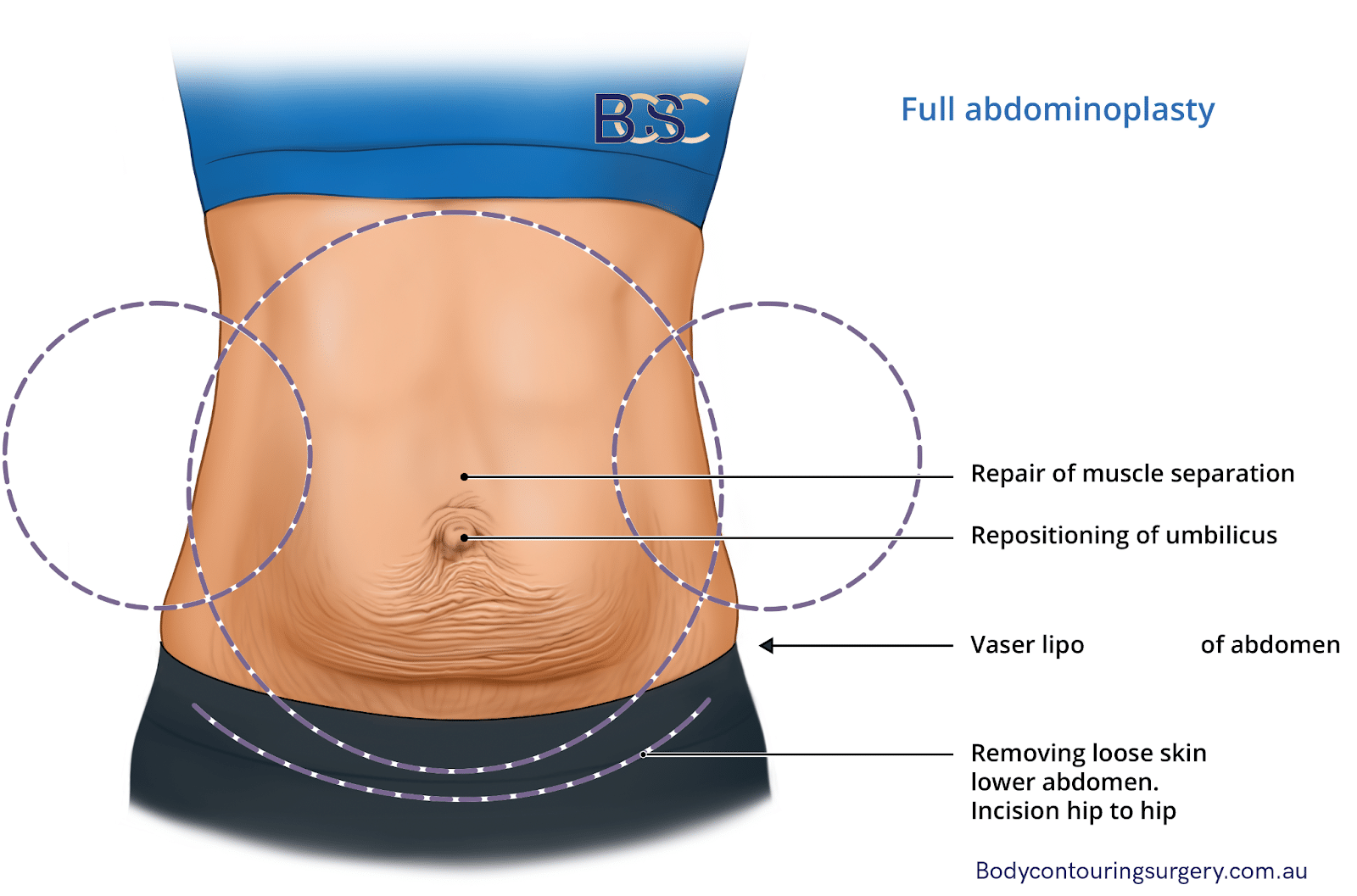
Fleur-de-Lis vs. Full Abdominoplasty
A full abdominoplasty is a standard procedure, addressing excess abdominal skin in the entire region, muscle repair, and belly button repositioning. However, unlike Fleur-de-Lis abdominoplasty, full abdominoplasty cannot adequately address skin laxity in the upper abdominal midsection, so it is generally unsuitable for massive weight loss patients.
In addition, since a full abdominoplasty is a standard abdominoplasty procedure, it requires only one horizontal incision, while Fleur-de-Lis abdominoplasty involves an additional vertical incision.
Benefits of Fleur-de-Lis Abdominoplasty
Fleur-de-Lis abdominoplasty offers several benefits, including:
- Creates enhanced and toned abdominal contour
- Repairs separated abdominal muscles
- Addresses significant excess skin on the lower abdomen and midsection
- Results in a smaller waist
Drawbacks of Fleur-de-Lis Surgery
Some of the drawbacks of Fleur-de-Lis abdominoplasty include:
- Longer recovery
- Extensive scarring
- Higher risk of wound infection
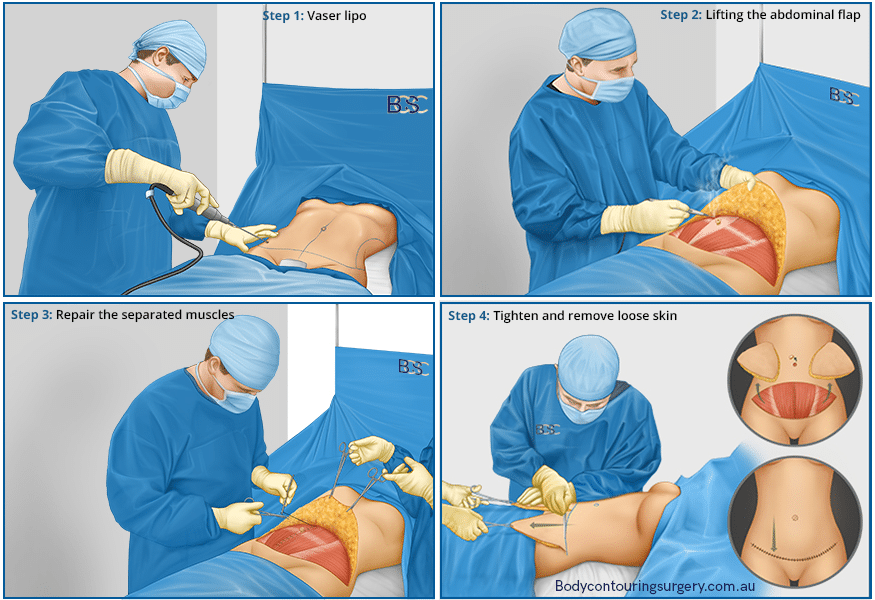
Surgery Guide: Fleur-de-Lis Abdominoplasty
Fleur-de-Lis abdominoplasty is a major surgery, performed under general anaesthesia, taking approximately four to five hours (or longer if liposuction or muscle repair are also involved.)
Surgery Preparation
Before the surgery, the specialist surgeon and patient review any last-minute queries and clarifications. The specialist surgeon reviews the potential risks and complications once again and advises the patient of the expected procedure time. The patient then consents to have the procedure.
Markings

Pre-Surgery markings of excess skin to be removed for fleur de lis abdominoplasty bending over | BCSC
While the patient is in the anaesthetic bay, the specialist surgeon marks the patient’s abdomen with a (indelible marker) A study published in the National Library of Medicine warns against using red pens. “Two volunteers ranked the top three most visible marker pens from each photograph. The results showed that Sharpie® W10 black, Dual Tip (Purple Surgical), and Easimark modern regular tip (Leonhard Lang) were the best performers across all skin types. Red pen should be avoided with a betadine skin preparation.” These markings serve as reference points, representing the excision area during the surgical procedures.

Pre-Surgery markings of excess skin to be removed for fleur de lis abdominoplasty bending over | BCSC
The first marking involves a standard abdominoplasty incision pattern, a horizontal marking running from hip to hip. An inferior vertical marking that runs along the upper abdomen’s midline is also indicated.
The vertical marking involves two lines resembling an inverted V. The specialist surgeon determines the base length of the V through a “pinch test.” In addition, the surgeon can round the inverted V to appear like an inverted U, increasing the excision site in instances requiring additional removal of upper abdominal skin.
The vertical and horizontal markings join at the groin area, creating an inverted T, resembling a three-petal lily flower.
Body Positioning on the Operating Table
After the marking, the patient lies in a supine position (on their back) on the operating table, ready for the operation.
Anaesthesia
Due to the procedure’s invasiveness, Fleur-de-Lis abdominoplasty surgery is performed with the patient under general anaesthesia. Administered by an anaesthetist, the anaesthesia sedates the patient so no pain, sensation, or memory of the fleur de lis procedure is experienced. Additionally, a tube is inserted in the patient’s breathing canal to facilitate breathing. The anaesthetist remains throughout the surgery to monitor the patient’s breathing, anaesthesia levels, and other vitals.
VASER Liposuction
Many specialist surgeons combine Fleur-de-Lis abdominoplasty surgery with liposuction to achieve optimal contouring. A specialised procedure that incorporates an advanced type of liposuction with Fleur-de-Lis abdominoplasty, VASER (Vibration Amplification of Sound Energy at Resonance) liposuction involves using ultrasound waves to break down, liquefy, and remove fat deposits in the body, allowing for easier extraction and enhanced results.
Though not all Fleur-de-Lis abdominoplasty patients require liposuction, VASER liposuction adds approximately one hour to the Fleur-de-Lis abdominoplasty procedure time.
VASER Liposuction Procedure performed as part of a fleur de lis abdominoplasty
Below is the procedure when VASER liposuction is involved.
Applying the Wetting Solution

Injecting wetting solution as part of VASER liposuction | BCSC
The specialist surgeon makes small incisions at the excision site, which allow the insertion of a hollow tube (cannula.) Using the cannula, the specialist surgeon applies a wetting solution to the fat tissue. A cannula system and pump help distribute the wetting solution evenly in the tissues.
The most commonly used wetting substance, tumescent fluid, which contains adrenaline, lignocaine, saline, and sodium bicarbonate, causes the tissue to swell up and become firm, allowing for more accurate fat removal with less bleeding.
Dr Beldholm notes that using a sufficient amount of the wetting solution enhances optimal results.
Protecting the Skin
During this procedure, the VASER probe oscillates at a very high frequency, causing it to become very hot. Therefore, it’s essential for the surgeon to protect the patient’s skin to prevent burns. Protective ports at the insertion points, a sufficient amount of fluid applied to the tissue, and wet cloths used to cover the naked skin are all protective measures the surgeon may utilise.
Fat Melting
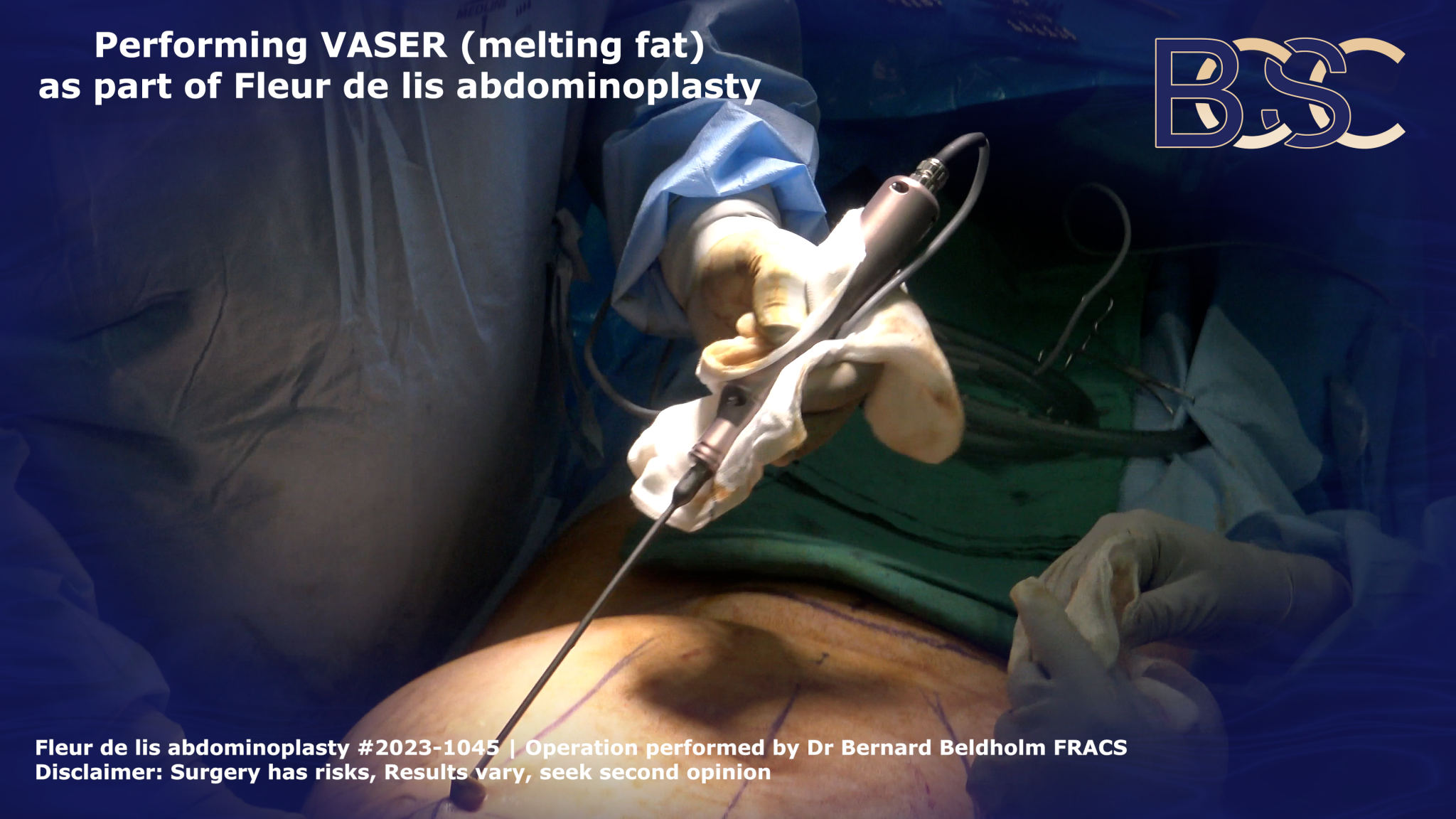
VASER as part of a fleur de lis abdominoplasty | BCSC
To melt the fat, the specialist surgeon inserts the VASER probe into the insertion points and moves it backward and forward. The VASER produces ultrasonic energy, forming bubbles in the wetting solution, dislodging, and emulsifying the fat.
When the fat is emulsified, the probe encounters less or no resistance as it moves through the fatty skin layer. This signifies that the fat is ready for removal. VASER liposuction ensures maximum abdominal fat melting and removal without damaging adjacent nerves, tissues, or blood vessels.
Fat removal

Liposuction as part of Fleur de lis abdominoplasty | BCSC
The abdominal fat removal process uses a machine to suck the fat through a cannula. Unlike traditional liposuction, which requires aggressive suction, the VASAR method involves the use of lower power because the fat is emulsified.
Belly Button Incision
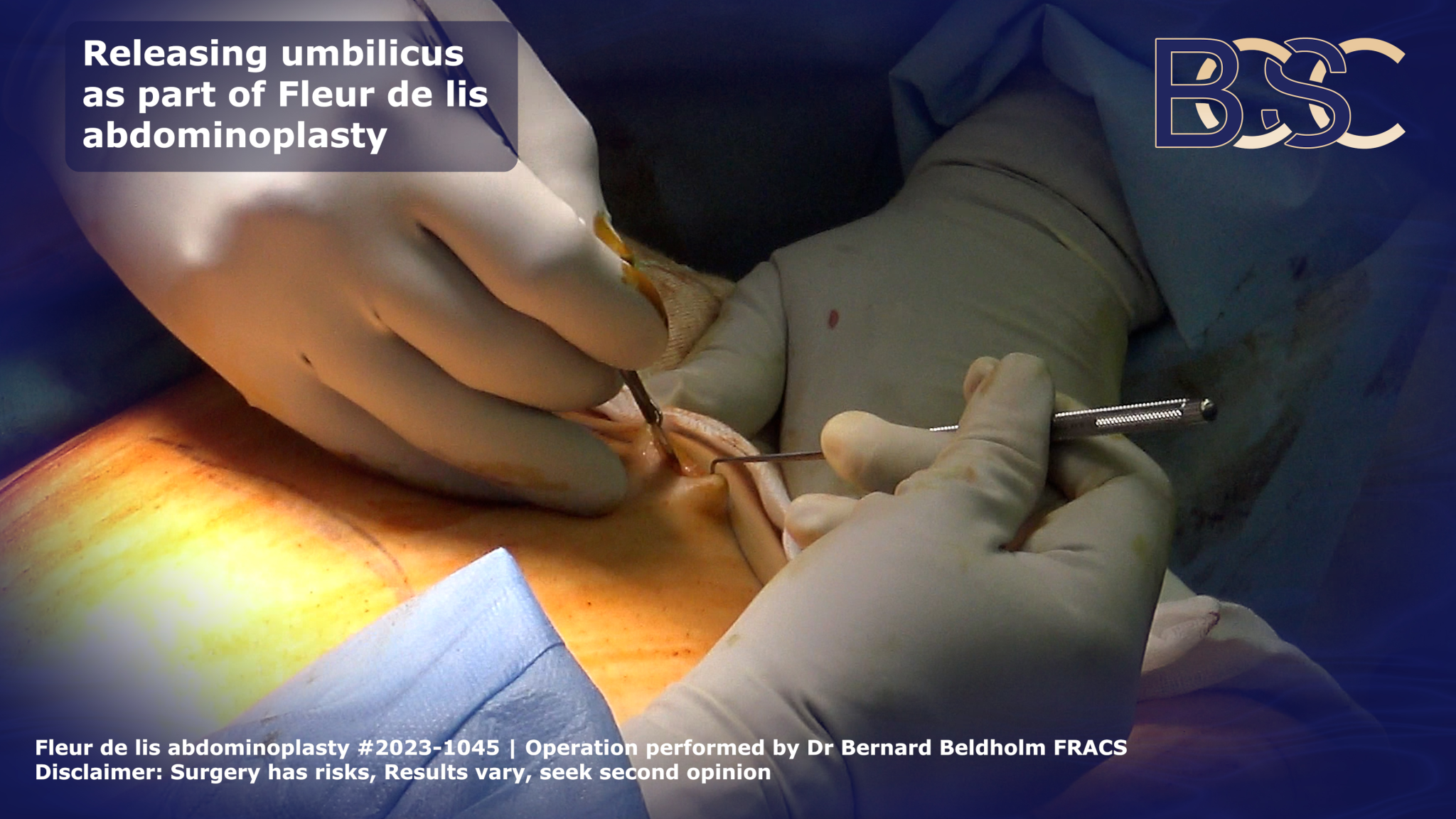
Incision around umbilicus in fleur de lis abdominoplasty | BCSC
The belly button is freed initially before the vertical part of the skin excess is removed. To free the belly button, an incision is made around the umbilicus, leaving the umbilical stalk fixed to the muscle. A surgeon’s assistant helps to stabilise the tissues adjacent to the belly button, preventing the tissues from moving during the procedure. By stitching a tiny plastic bit onto the umbilical stack, the surgeon is able to locate the belly button later in the procedure.
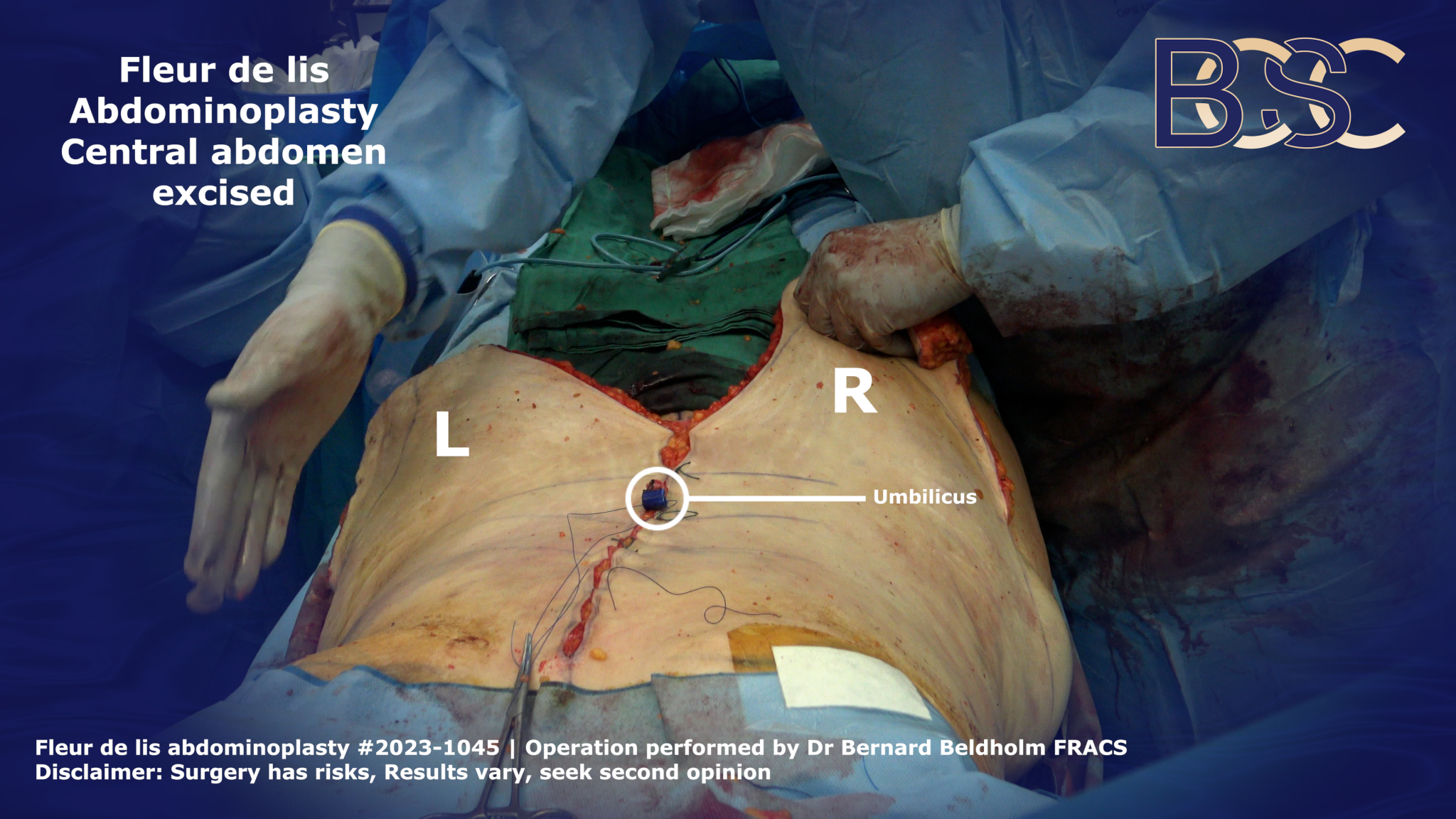
Vertical Incision

Excision of central abdominal skin in Fleur de lis abdominoplasty | BCSC
A vertical incision helps in removing loose skin around the patient’s midsection.
The specialist surgeon follows the markings, creating an inverted V vertical incision. Any open blood vessels are sealed using diathermy, reducing bleeding and maintaining hemostasis. The surgeon then frees the excess loose skin from the underlying tissue.
Removing the Loose Skin
To ensure the removal of the exact amount of excess skin, the specialist surgeon performs a trial by gathering the skin at the midline and securing it with sutures. Some surgeons may use clips instead of sutures. However, securing the excess skin in place using clips can be challenging. The specialist surgeon then marks the excess skin to be removed.
Closing the Incision
Vertical incision closed in Fleur de lis abdominoplasty | BCSC
The vertical incision closure is done in layers, starting from the deeper layers and moving towards the skin surface. The surgeon uses absorbable sutures for the progressive layer closure.
Dr Bernard uses ARTISS tissue glue to ensure the incision is perfectly closed as it helps reduce the risk of seroma, a major post-surgical complication.
Horizontal Incision
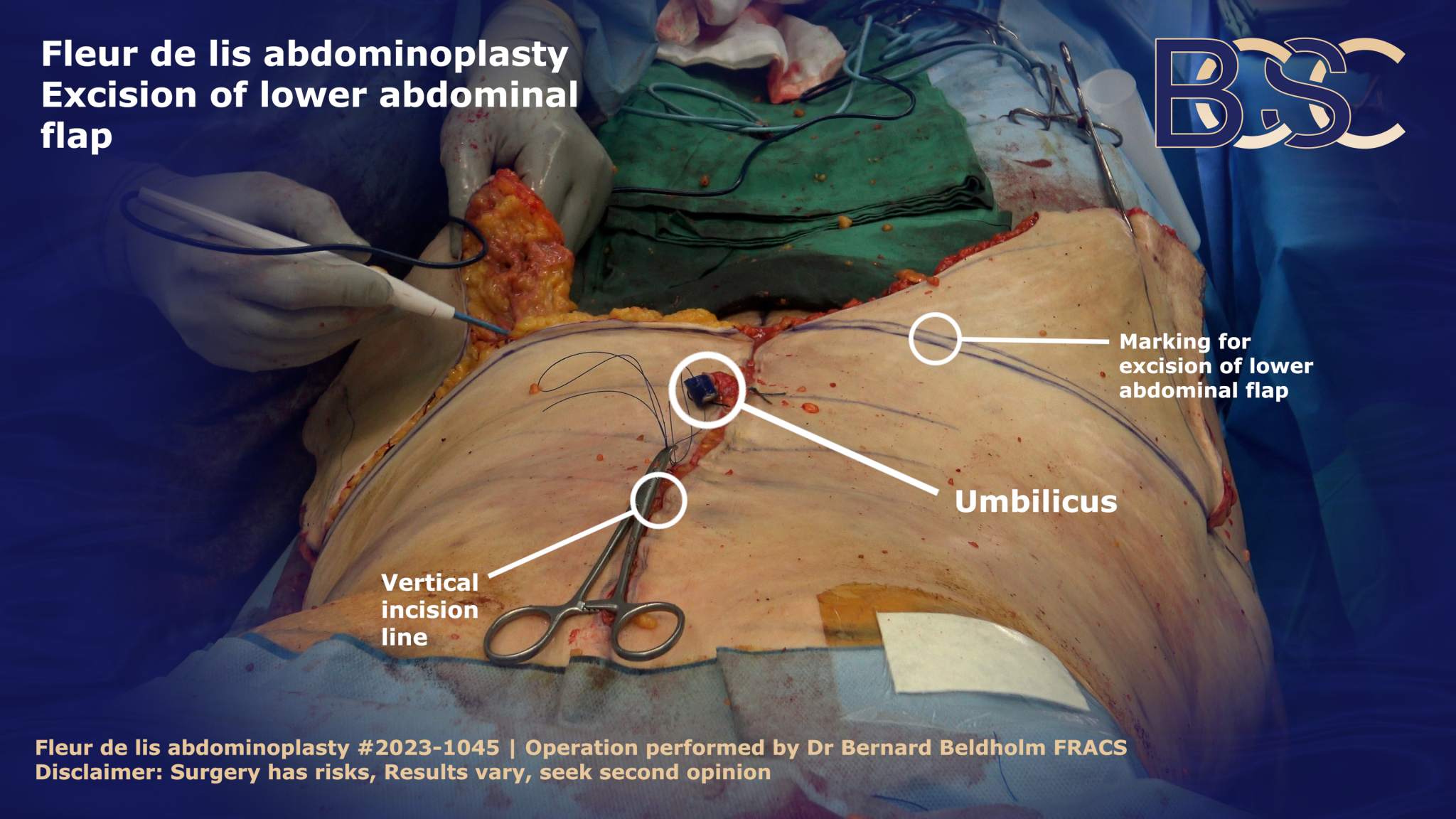
Excision of lower abdominal flap in Fleur de lis abdominoplasty | BCSC
After the vertical incision, the next step involves creating a horizontal, standard tummy tuck incision. The incision helps address the remainder of the excess skin, particularly in the lower abdomen.
The horizontal incision runs from hip to hip along the lower abdomen. The specialist surgeon will make the incision using the initial markings as a reference. The process also involves subsequent closure of any blood vessels that open during the process. This helps reduce bleeding as the surgeon frees the skin from the underlying tissues. The horizontal incision goes just below the Fascia of Scarpa but not further.
The Fascia of Scarpa appears white, making it easily visible during dissection. Dr. Beldholm avoids dissecting past the Fascia of Scarpa to preserve the nerves, lymphatics, and blood flow. This also reduces the need for surgical drains that remove excess fluid from a surgical wound, preventing its accumulation.
Muscle Repair
The specialist surgeon repairs the separated abdominal muscles by suturing along the midline. Dr Beldholm uses a V-Loc barbed suture, which hooks onto the tissues, eliminating knotting common with regular sutures. The lack of knots reduces the time the patient is under general anaesthesia. In addition, it ensures the patient doesn’t feel the sutures under their skin.
Belly Button Repositioning
Since Fleur-de-Lis abdominoplasty removes significant abdominal skin and fat, the belly button requires repositioning. The process requires expertise to ensure the belly button looks natural, not sitting too high or low on the abdomen.
The belly button is sutures into the vertical extent of the incision as part of the final closure.
Closing the Incision
The last part of the surgical procedure involves closing the incision. 2/0 vicryl sutures are used for the Fascia of Scarpa, which can withstand tension without jeopardising vascularity. Barbed sutures are used for the superficial abdominal layers, and the overlying tissues are then closed using absorbing sutures and ARTISS tissue glue.
Finalising Your Surgery
At this point, the cosmetic surgery is almost complete.
Wound Dressings

PICO wound dressing | BCSC
Dr. Beldholm uses PICO negative pressure wound therapy (NPWT) an advanced surgical dressing for wounds. The PICO dressings have a battery pack, which allows it to exert negative pressure on the wound when powered on. This promotes blood circulation, optimising wound healing and recovery process. The dressings also reduce the risk of wound infection.
Patients have the PICO dressings removed after seven to ten days.
Compression Garments
After wound dressing, compression garments are applied. Compression garments help reduce seroma and swelling. Patients are advised to wear compression garments for four to six weeks.
Results
It takes approximately twelve months for residual swelling to subside and full results to become visible. However, Fleur-de-Lis scars may take up to two years to fade. It’s important to note that patients recover differently, and individual results vary.
Fleur-de-Lis Abdominoplasty Surgery Recovery
Fleur-de-Lis abdominoplasty surgery aftercare is essential for optimal results. After surgery, the specialist surgeon will provide the patients with post-op information to aid in Fleur-de-Lis abdominoplasty surgery recovery.
After surgery, most patients are concerned about how much time they will have to stay in the hospital, as well as how long it will take until they are able to resume their normal daily activities, including working, bathing, driving, and exercising.
Remaining in the Hospital Following Fleur-de-Lis Abdominoplasty

Most surgeons recommend that Fleur-de-Lis abdominoplasty patients spend approximately four to ten days after surgery in the hospital for further observation.
Showering After Fleur-de-Lis Abdominoplasty
It’s not advisable to shower immediately after surgery. Specialist surgeons recommend showering a day or two after surgery.
Time off from Working, Exercising, and Driving After Fleur-de-Lis Abdominoplasty
Patients should take two to four weeks off work to enhance recovery. However, most patients can resume their normal activities after three weeks and fully exercise after six to eight weeks.
Is Fleur-de-Lis Abdominoplasty Surgery Painful?
Patients will experience intense pain during the first two days after surgery. The doctor will prescribe painkillers to manage the pain but the pain gradually subsides.
Possible Risks and Complications of Fleur-de-Lis Abdominoplasty Surgery
Due to its invasiveness, Fleur-de-Lis abdominoplasty poses several risks, considered comparable to those of traditional abdominoplasty.
- Seroma
- Necrosis
- Blood clots
- Hematoma
- Poor scarring
- Nerve damage
- Uncontrolled bleeding
- Poor reaction to anaesthesia
- Undesirable cosmetic result that requires a revision
- Wound infection
- Loss of skin sensation
- Asymmetry
Other risks are also possible. Consult a specialist general surgeon for more information.
Bottom Line
Undergoing a Fleur-de-Lis abdominoplasty is a major decision for most patients. Therefore, understanding the process, including the recovery and risks, is key. The above Fleur-de-Lis operation guide reviews everything a patient is required to know before undergoing a Fleur-de-Lis abdominoplasty.
References
- Hoyos, A. E., & Millard, J. (2007). VASER-assisted high-definition liposculpture. Aesthetic Surgery Journal, 27(6), 594–604.
- Yazar, S. K., & Serin, M. (2019). Comparison of Aesthetic Quality of the Final vertical Scar in Abdominoplasty with Conventional and Mini Inverted t-Scar. Medicina, 55(5).
- Friedman, T., Coon, D., Michaels, J., Purnell, C. A., Hur, S. H., Harris, D. N., & Rubin, J. P. (2010). Fleur-de-Lis abdominoplasty: A safe alternative to traditional abdominoplasty for the massive weight loss patient. Plastic and Reconstructive Surgery, 125(5), 1525–1535.
- Chen, E., Kao, C., & Ku, H. (2023). Fleur-de-Lis Mini Abdominoplasty Access in Radical Resection of a Large Abdominal Wall Desmoid Tumor. Plastic and Reconstructive Surgery Global Open, 11(10).
- Mitchell, R. T., & Rubin, J. P. (2014). The Fleur-de-Lis abdominoplasty. Clinics in Plastic Surgery, 41(4), 673–680.
- Ziegler, U. E., Ziegler, S. N., & Zeplin, P. H. (2017). Modified Fleur-de-Lis abdominoplasty for massive weight loss patients. Annals of Plastic Surgery, 79(2), 130–134.
- Dellon, A. L. (2019). Fleur-de-Lis abdominoplasty. Aesthetic Plastic Surgery, 9(1), 27–32.
- De Souza Pinto, E. B., De Souza Pinto Abdala, P. C., Maciel, C. M., De Paula Turchiari Dos Santos, F., & De Souza, R. P. M. (2006). Liposuction and VASER. Clinics in Plastic Surgery, 33(1), 107–115.
- Michalska, A., Rokitaⴕ, W., Wolder, D., Pogorzelska, J., & Kaczmarczyk, K. (2018). Diastasis recti abdominis — a review of treatment methods. Ginekologia Polska, 89(2), 97–101.
- Kißler, H., & Settmacher, U. (2013). Bariatric surgery to treat obesity. Seminars in Nephrology, 33(1), 75–89.
- Gibas-Dorna, M., Szulińska, M., Turkowski, P., Kupsz, J., Sowińska, A., Mikrut, K., Bernatek, M., & Piatek, J. (2017). The Effect of VASER Abdominal Liposuction on Metabolic Profile in Overweight Males. American Journal of Men’s Health, 11(2), 284-293.
- Vidal, P., Berner, J. E., & Will, P. A. (2017). Managing Complications in Abdominoplasty: A Literature Review. Archives of Plastic Surgery, 44(5), 457-468.
![Are You a Candidate for Arm Lift Surgery? [Brachioplasty]](https://bodycontouringsurgery.com.au/wp-content/uploads/2023/07/BCSC_Ideal_candidates_for_brachioplasty-featured_image-1.jpg)
