Getting Medicare to Cover Your Abdominoplasty, What are the Rules?
Like many other surgical procedures, abdominoplasty (tummy tuck) can be expensive to fund. Therefore, most patients turn to Medicare rebates to help fund abdominoplasty and other surgical procedures. However, Australia’s Medicare has strict criteria regarding the coverage of surgical procedures, and patients must meet all the listed requirements.
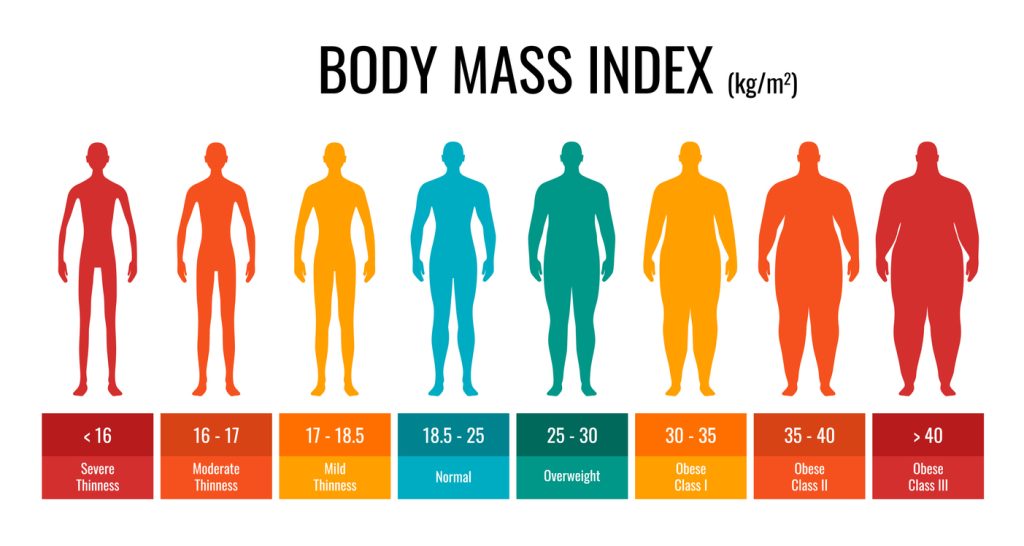
There are two types of abdominoplasties that qualify for an MBS item number. The first type is post-pregnancy, with muscle separation and resulting symptoms. The second type is post-weight loss, with a weight loss of more than 5 BMI levels and stable weight for at least 6 months. This type is applicable when the skin is causing significant problems.

Medicare offers different MBS item numbers for medicare rebate abdominoplasty options. However, this will depend on the symptoms, degree of weight loss, and medical condition. There’s no need to panic if you are considering abdominoplasty in Newcastle or Sydney and don’t know if you can get Medicare coverage. Read on to learn to find everything related to tummy tuck and Medicare rebates.
What is the Medicare Benefits Schedule?

The Medicare Benefits Schedule (MBS) lists medical services by the Australian government qualifying for rebates under Medicare. The MBS contains item numbers, known as MBS item numbers, for different medical procedures. This means a patient must have an MBS item number for a particular procedure to qualify for Medicare rebates.
How Does Medicare and Private Health Insurance Work in Australia?
Medicare funds operations that are considered medically necessary. MBS assigns each operation an MBS item number, and each number has specific criteria that each patient must fulfil. If you have a MBS item number for your procedure, then you will get money back from Medicare.
Medicare assigns a 100% fee for each of the Medicare numbers, and you will get a 75% rebate for in-hospital medical services. Hospital cover funds the remaining 25%. Note that Medicare does not cover the hospital costs.
Medicare has not increased for ten years; therefore, having private insurance is essential. Private health insurance will also cover the hospital costs if you have the correct coverage. Health funds pay a minimum of 100% of the MBS fee, but many pay more. Health funds don’t pay for outside-the-hospital medical services, like visiting your GP, but Medicare covers 85% of the MBS fee on these services.
Some terms concerning private health funds include a No Gap and a Known Gap. This is the extra amount a patient needs to pay from their pocket to cover the extra fees above the MBS fees.
No-Gap: The doctor accepts whatever Medicare or the health fund pays. However, given that the fees have not increased for more than ten years, these fees would not even cover the running cost of a practice.
Known Gap: Private health insurance mandates a specific gap that is allowed. However, this is still significantly lower than the usual costs for running a practice, and it’s not sustainable for most plastic surgeons.
Will Medicare Cover My Abdominoplasty Cost?
Getting a Medicare rebate will provide you with some financial relief. However, you will only be eligible for Medicare rebates if you undergo an abdominoplasty to treat a medical condition and not as a cosmetic surgery. Medicare does not offer rebates for cosmetic procedures. An abdominoplasty can be a cosmetic or a medical operation (medical necessity).
You will not qualify for an MBS item number if you have loose skin and dislike how your abdomen looks but have no medical symptoms necessitating the operation.
However, you may qualify for an MBS item number if you have significant weight loss and have medical issues with loose skin. You’ll also be eligible if you experience significant muscle separation causing medical symptoms after pregnancy.
Medicare will only cover a small portion of the total cost, and the patient will fund the rest. The additional costs include anaesthesia and specialist plastic surgeon fees. Patients should note that no public hospitals offer free cosmetic surgery in Australia.
Note Medicare rebate criteria change with time. Before 2016, Medicare covered tummy tucks for women who had experienced pregnancy. However, it was scrapped, and the Australian government only reinstated Medicare benefits for abdominoplasty patients undergoing massive weight loss, not pregnancy-related. For women who have experienced pregnancy, the weight loss calculation involves pre-pregnancy weight, not weight directly associated with the pregnancy. Women with significant muscle separation (diastasis recti) may also be eligible for an MBS item number.
How To Be Eligible for Tummy Tuck (Abdominoplasty) Medicare Coverage
Medicare only covers tummy tuck (abdominoplasty) procedures if it’s deemed medically necessary. The patient must qualify for a Medicare Item Number under the Medicare Benefits Schedule.
If you have Medicare coverage, the first step is to get a GP’s (General Practitioner) referral. The GP provides critical information regarding your condition. Ensure you notify the GP of all symptoms to solidify evidence proving medical necessity.
You must get a GP referral before booking an abdominoplasty consultation with a specialist surgeon. The referral is valid for twelve months and is crucial in claiming an abdominoplasty Medicare rebate.

The specialist surgeon uses this information to assess your eligibility and see if the condition qualifies as a medical necessity. The specialist surgeon must determine if you qualify for an MBS item number. The surgeon then assigns a MBS item number you will get in your quote. If the surgeon does not follow the correct criteria, Medicare can charge them with medicare fraud.
After getting an MBS item number, check with your health fund if they cover the procedure or not. Ensure to review your health care policy to ensure coverage for cosmetic surgical procedures. Note that you will need to pay the surgeon’s fee prior to the surgery. Once you have surgery, you can claim the money from your health fund.
You do not have to claim the rebate from Medicare; you only claim from a private health fund. The private health fund will then claim 75% of the MBS fee from Medicare on your behalf. The hospital would also bill your health fund directly for the cost of the operation.
The factors necessary to prove medical necessity for your abdominoplasty include significant weight loss (around five or more MBI points) within a short period, skin rashes and other infections, incontinence, abdominal muscle separation (rectus diastasis), and hernias.
Also, you must meet several conditions if considering tummy tuck surgery (abdominoplasty) due to post-pregnancy concerns. These include proving that other non-surgical conservative treatments haven’t worked, that you have maintained a stable weight for at least six months, and proof of medical necessity. Medicare doesn’t offer abdominoplasty coverage if the primary goal is to remove excess skin resulting from pregnancy.
Let’s look deeper at some medical necessity factors to ensure you get available Medicare rebates.
Show Significant Weight Loss and Maintain a Steady Weight
Prior to pregnancy, you must have substantial weight loss of at least 5 BMI points, around ten to fifteen kgs. You must also not have had weight fluctuations for at least six months. Minimal weight fluctuations but within a steady range are allowed.
Have Excess skin that is affecting your daily life
Excess skin can result from massive weight loss. Excess redundant abdominal skin can be hard to clean between the folds, allowing sweat and bacteria to accumulate. This can lead to skin rashes and infections. In addition, chafing as the skin rubs against itself may result in skin redness, irritation, and painful sores.
Patients with excess skin affecting their daily lives can qualify for a Medicare rebate on abdominoplasty. However, the patient must prove they have tried other conventional non-surgical methods without success for at least three months.
Hernias
Hernias result from a tear in the abdominal wall and can be very painful. Abdominoplasty helps reduce the hernia and reduces the risk of its reoccurrence. The doctor can administer pain medication before further treatment. Patients with hernias and the doctor can prove using ultrasound can qualify for a Medicare benefit on a tummy tuck procedure.
MBS Item Numbers for Tummy Tuck (Abdominoplasty) Surgery
Medicare provides rebates if you can prove, through documented symptoms, that the abdominoplasty procedure satisfies the muscle repair and weight loss criteria.
Here are MBS item numbers that reimburse for different tummy tuck surgeries. Depending on the type and severity of surgery, the patient may be eligible for partial or full MBS number coverage.
MBS Item Number 30166
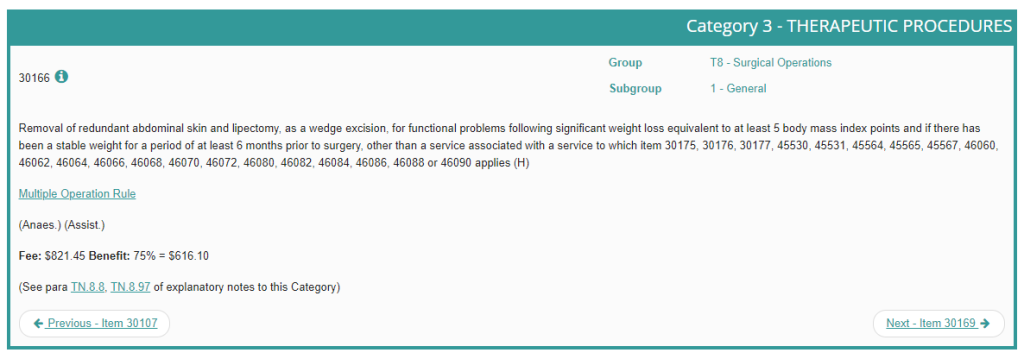
Removal of redundant abdominal skin and lipectomy as a wedge excision. This is for functional problems following significant weight loss equivalent to at least five body mass index points. It’s also helpful if there has been a stable weight for at least six months before surgery.
MBS Item Number 30169
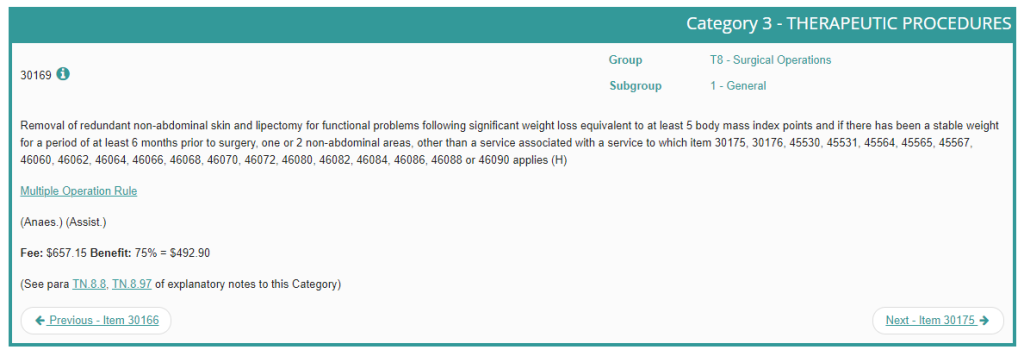
Removal of redundant non-abdominal skin and lipectomy. It applies to functional problems following significant weight loss equivalent to at least five body mass index points. It is also applicable if there has been a stable weight for at least six months prior to surgery in one or two non-abdominal areas.
MBS Item Number 30175
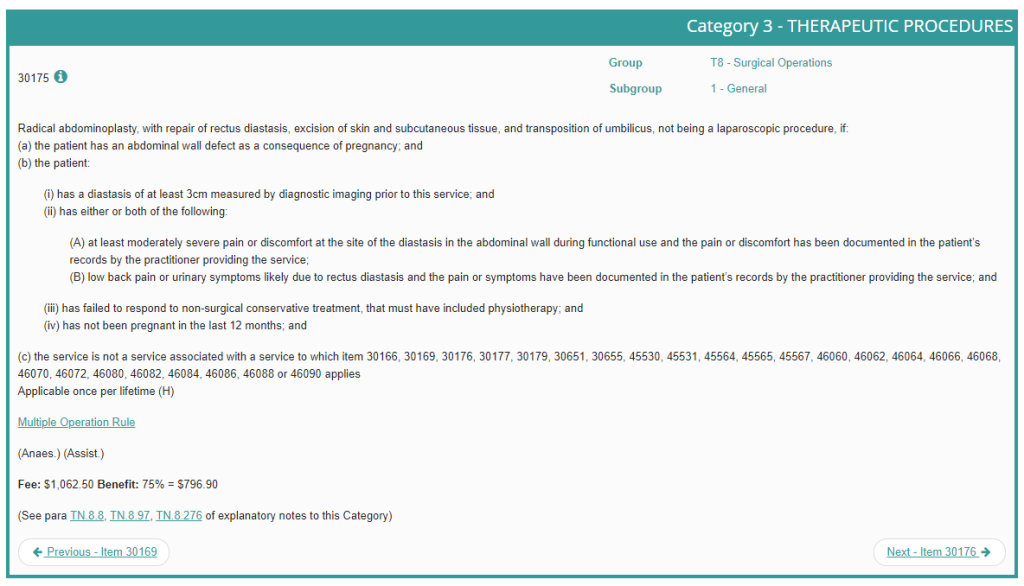
It’s a new Medicare item number introduced on 1st July 2022, which caters to muscle repair (diastasis recti) after pregnancy. It’s a radical tummy tuck involving rectus diastasis repair, skin and, subcutaneous tissue excision, and transposition of the umbilicus. For eligibility, patients must meet the following criteria:
- Have a diastasis recti of at least 3cm measured by diagnostic imaging prior to this service
- Have symptoms of at least moderate severity of pain or discomfort. These symptoms should be at the site of the diastasis in the abdominal wall during functional use and/ or low back pain. Pain or urinary symptoms likely due to rectus diastasis must have been recorded. The practitioner providing this service has documented these symptoms in the patient’s records for ** symptomatic management.
- Have failed to respond to non-surgical conservative treatment, including physiotherapy
- Not have been pregnant in the last 12 months
MBS Item Number 30177
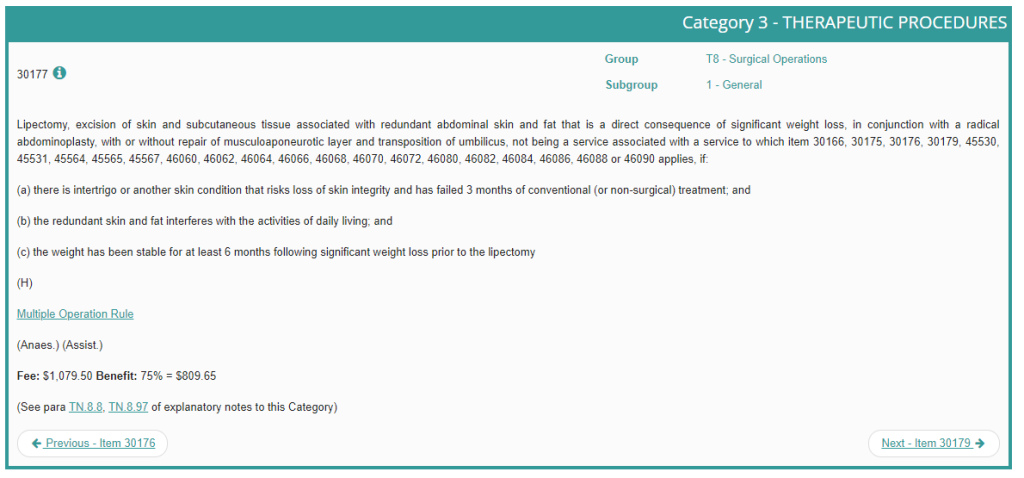
It involves lipectomy, excision of skin and subcutaneous tissue associated with redundant abdominal skin and fat that is a direct consequence of significant weight loss, in conjunction with a radical abdominoplasty, with or without repair of musculoaponeurotic layer and transposition of the umbilicus. The item number caters to weight loss, and it’s applicable if:
- There is intertrigo or another skin condition that risks the loss of skin integrity.
- The condition has failed three months of non-surgical treatment
- The redundant skin and fat interfere with daily living activities
- The patient has had stable weight for at least six months following significant weight loss prior to the lipectomy
- The patient has a hernia, which can be documented in an ultrasound
MBS Item Number 30179
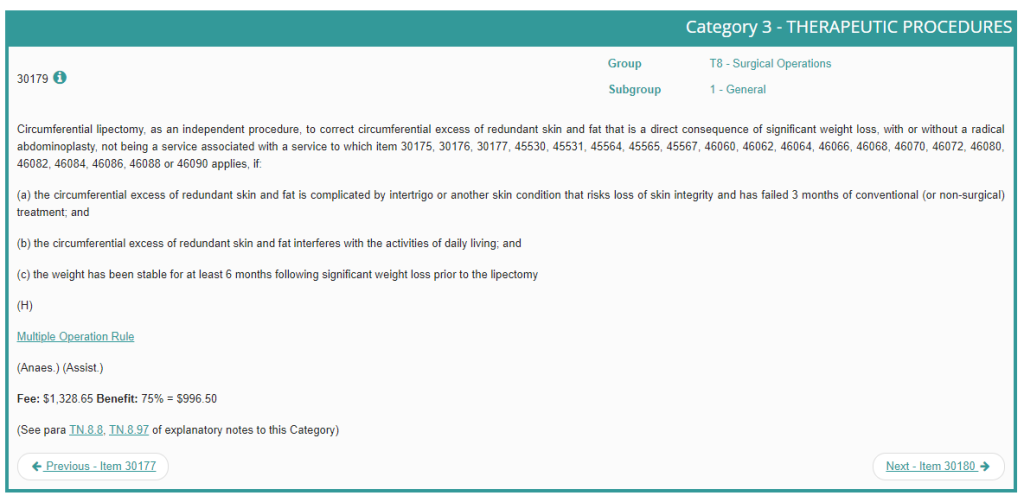
- As an independent procedure, it involves circumferential lipectomy to correct circumferential excess of redundant skin and fat, a direct consequence of significant weight loss. It applies if:
- There is intertrigo or another skin condition that risks the loss of skin integrity
- The condition has failed three months of non-surgical options
- The redundant skin and fat interfere with daily living activities
- The patient has had stable weight for at least six months following significant weight loss before the lipectomy
Standard Requirements for Abdominoplasty-Related MBS Item Numbers
As noted, each item number has its requirements. However, there are common criteria for all the item numbers. These include,
- Lipectomy is not intended as a primary bariatric procedure to correct obesity.
- MBS benefits are not available for surgery performed for cosmetic purposes
- Need to have had significant weight loss (SWL). SWL is defined as a weight loss equivalent of at least five BMI units.
- Weight must be stable for at least six months following significant weight loss before lipectomy.
- For significant weight loss that has occurred following pregnancy, the products of conception must not be included in the calculation of baseline weight to measure weight loss against
Bottom Line
Funding an abdominoplasty procedure can be challenging, and Medicare rebates can help ease the financial burden. However, Medicare covers abdominoplasty if it’s a medical necessity and not for cosmetic purposes. Therefore, to qualify for Medicare rebates, a patient must prove, using documented symptoms, that they meet the weight loss or muscle repair criteria under Medicare. Above, find the MBS item numbers that allow a patient to claim rebates on an abdominoplasty procedure.
References
- Dietz, U., Menzel, S., Lock, J. F., & Wiegering, A. (2018). The treatment of incisional hernia. Deutsches Arzteblatt International.
- Regan JP, Casaubon JT. Abdominoplasty. [Updated 2023 Jul 24]. In: StatPearls Treasure Island (FL): StatPearls Publishing; 2023 Jan.
- Simons, M. P., Śmietański, M., Bonjer, H. J., Bittner, R., Miserez, M., Aufenacker, T. J., Fitzgibbons, R. J., Chowbey, P., Tran, H., Sani, R., Berrevoet, F., Bingener, J., Bisgaard, T., Bury, K., Campanelli, G., Chen, D. C., Conze, J., Cuccurullo, D., De Beaux, A. C., . . . Wijsmuller, A. R. (2018). International guidelines for groin hernia management. Hernia, 22(1), 1–165.
- Nb, S., Wc, H., Mills, S. D., Rajashekara, B., Taylor, Nb, T., Young, H., & Kivuls, J. (2008). Abdominal Lipectomy: A Prospective Outcomes Study. The Permanente Journal, 12(2), 23–27.
- Aly, A., & Mueller, M. (2014). Circumferential truncal contouring. Clinics in Plastic Surgery, 41(4), 765–774.
- Michalska, A., Rokita, W., Wolder, D., Pogorzelska, J., & Kaczmarczyk, K. (2018). Diastasis recti abdominis — a review of treatment methods. Ginekologia Polska, 89(2), 97–101.
- Jensen, J. A. (2007). Medical ultrasound imaging. Progress in Biophysics & Molecular Biology, 93(1–3), 153–165.