Fleur De Lis Abdominoplasty Complications Post Weight Loss: Evidence-Based Insights from Recent Studies
Our Specialist General Surgeons (FRACS) provide reconstructive and body contouring surgery for patients after significant or massive weight loss. This educational article reviews current evidence on Fleur-de-Lis abdominoplasty complications post weight loss, offering a comprehensive view of outcomes, risk factors, and treatment options. Individual results vary, and all surgery carries risks.
Understanding the Fleur-de-Lis Abdominoplasty

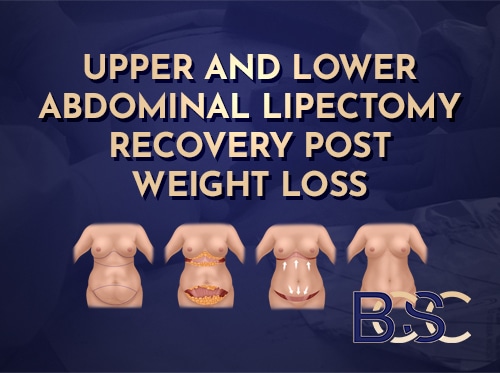
A Fleur-de-Lis abdominoplasty (commonly referred to as a Fleur-de-Lis tummy tuck) is a major reconstructive surgery within the field of plastic surgery performed to remove excess skin and tighten the abdominal wall following significant weight loss. It is generally considered for post-bariatric surgery patients or individuals who have achieved massive weight loss through lifestyle change, diet, or weight management medication. After fleur de lis surgery, maintaining a stable weight and a healthy lifestyle is crucial to preserving surgical results and minimising risks.
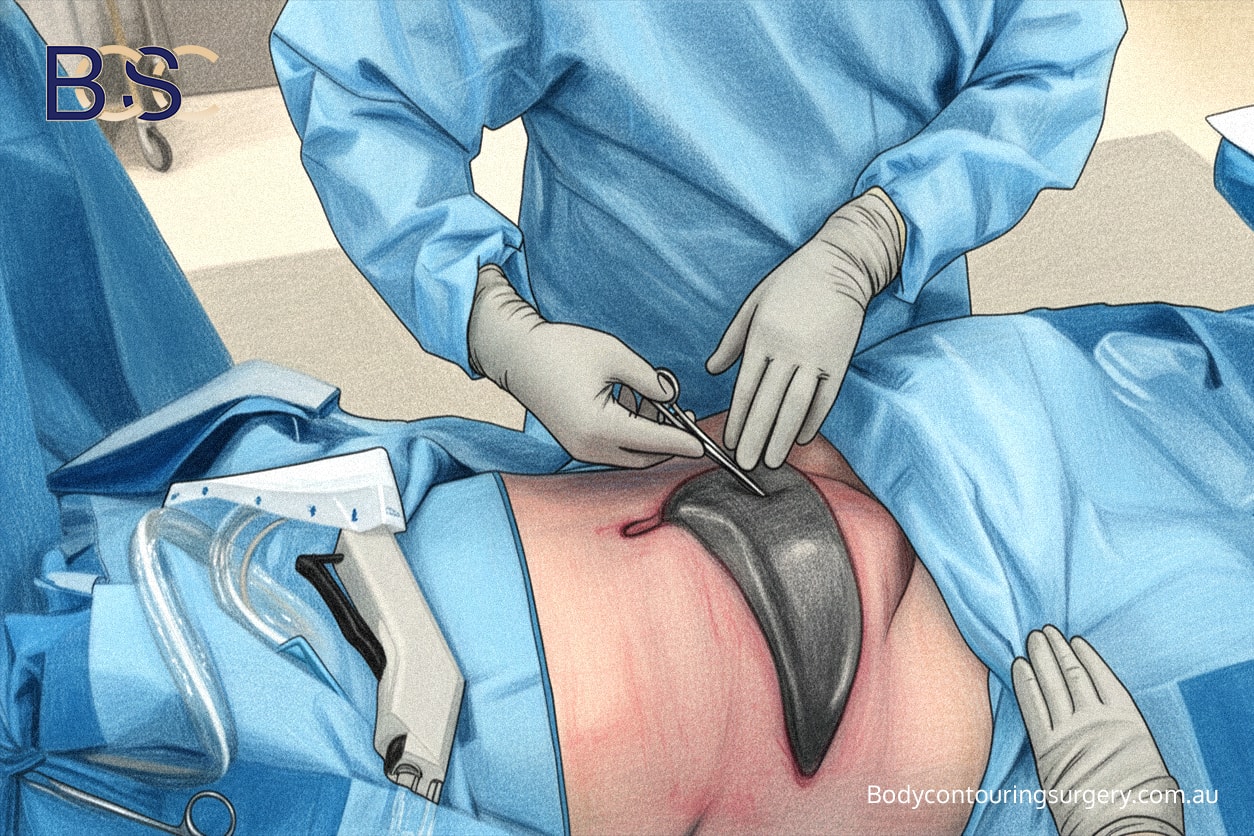
This body contouring surgery differs from traditional abdominoplasty because it removes excess abdominal skin in two directions — vertically and horizontally. The vertical incision forms an inverted-T or fleur-de-lis pattern, which enables greater skin tightening and correction of both horizontal and vertical laxity. This technique can also repair separated abdominal muscles (diastasis recti) and support to the abdominal wall.
While beneficial for post bariatric patients, the Fleur-de-Lis approach is a major surgery that carries recognised risks such as bleeding, seroma, and wound infection. Understanding potential complications allows patients and surgeons to plan for recovery and informed decision-making.
Why Fleur-de-Lis Abdominoplasty After Weight Loss Surgery?

Bariatric surgery
After bariatric surgery such as gastric bypass or sleeve gastrectomy, many patients experience significant excess skin in the abdominal region. This loose abdominal skin can lead to irritation, rashes, or difficulty with hygiene and clothing.
This technique provides more comprehensive correction of redundant skin and allows abdominal muscle tightening. However, because of the additional vertical scar, patients face a higher risk of wound healing problems at the incision junction.
This operation may be performed alongside other body contouring procedures such as thigh lift Thighplasty), or liposuction (suction-assisted lipectomy). These combined procedures require careful planning to ensure adequate healing and minimise postoperative complications.
Pre-Surgical Preparation and Risk Factor Analysis

Stable weight before surgery
Before abdominoplasty surgery, patients undergo a detailed medical evaluation to identify risk factors that may influence outcomes. Achieving a stable weight for at least six months helps prevent wound tension and recurrence of skin laxity. Maintaining a healthy diet and correcting nutritional deficiencies are essential steps before surgery, especially for bariatric surgery patients.
Key Preoperative Considerations
Pre-surgical planning
- Stable weight: Reduces tissue stress and promotes smoother healing.
- Nutritional optimisation: Sufficient protein, zinc, and vitamins A and C support collagen formation and wound healing.
- Smoking cessation: Stopping smoking decreases the risk of wound breakdowns.
- Medical control: Conditions such as diabetes or cardiovascular diseases should be well-managed to support recovery.
- Realistic expectations: Patients should understand that outcomes vary.
Evidence from Plastic and Reconstructive Surgery Studies
Applying VAC dressing for wound breakdown
Research published in Plastic and Reconstructive Surgery, Ann Plast Surg, and the Aesthetic Surgery Journal provides data on Fleur-de-Lis abdominoplasty complications post weight loss. Many clinical studies specifically focus on fleur de lis abdominoplasty, examining patient selection, surgical technique, and outcomes, especially in individuals with significant weight loss or excess tissue.
Parsa et al. (1) reviewed 55,596 cases and reported a major complication rate of 2.1%, including haematoma (0.7%), wound infection (0.6%), and deep vein thrombosis (0.18%).
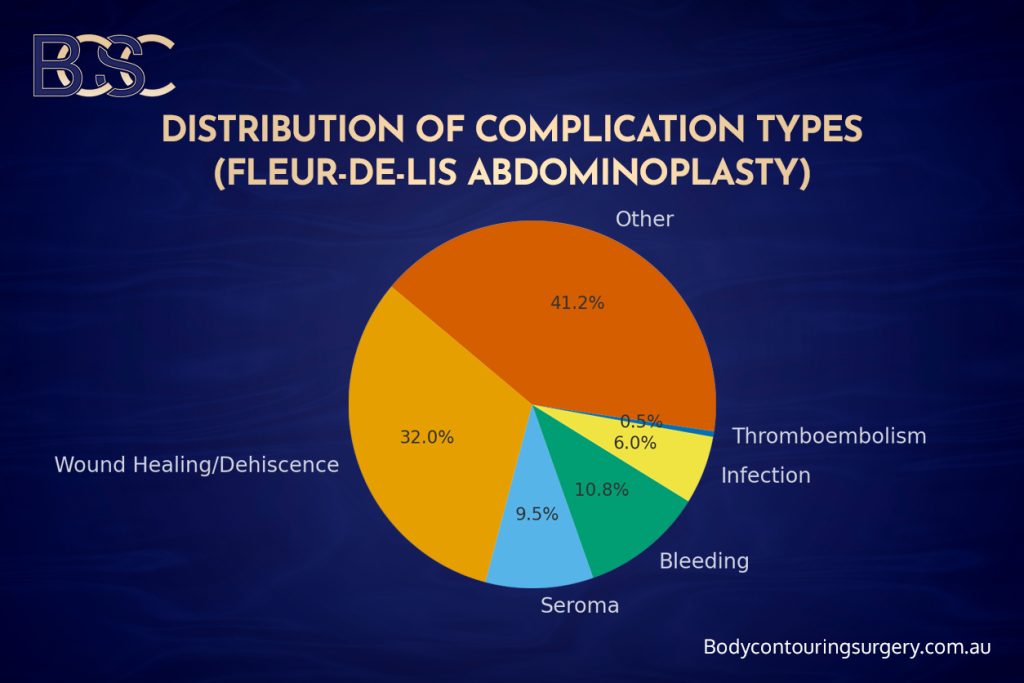
Distribution of surgical complications in Fleur de lis abdominoplasty
Sommer et al. (2) analysed 406 post bariatric abdominoplasty patients, showing total complication rates of 41.9%, with wound issues (32%) and seroma (9.5%).
Further evidence from Br J Plast Surg and J Plast Reconstr Aesthet Surg indicates that while minor complications are more common, they are generally manageable with conservative care (3,4). These studies highlight that risk factors such as age, BMI, and tissue resection weight influence outcomes more than surgical technique alone.
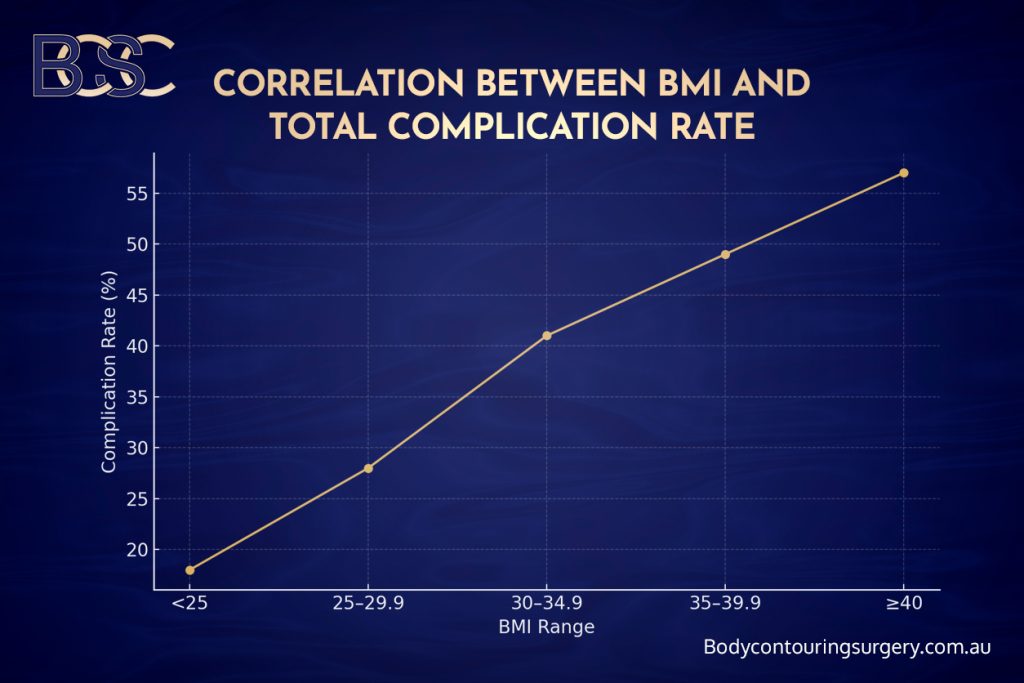
Correlation of BMI and total complication rate
Common Complications and Management Options
Understanding the potential complications associated with Fleur-de-Lis abdominoplasty is crucial for patient education and informed consent. This section outlines the most frequently reported issues encountered after surgery, explaining their underlying causes, how they can be prevented, and what treatment options are available. The aim is to provide patients and readers with a balanced and realistic understanding of the recovery process. By learning about these complications, individuals can recognise early warning signs, communicate promptly with their surgical team, and take appropriate steps to support effective healing.
Haematoma

Haematoma
A haematoma is a collection of blood beneath the skin that can lead to swelling, bruising, or discomfort following surgery. This occurs when small blood vessels leak after the operation. Patients may notice a firm or tender area beneath the incision.
Causes: Hypertension, physical strain too soon after surgery, or coagulation abnormalities.
Prevention: Careful surgical haemostasis, use of drains, and avoidance of early strenuous activity.
Management: Small haematomas are treated with cold packs, and observation. Large or expanding haematomas require urgent surgical evacuation and haemostasis. Monitoring haemoglobin levels is essential, and blood transfusion may be required if blood loss is significant.
Seroma
A seroma is the accumulation of clear serous fluid beneath the skin flap and remains one of the most frequent postoperative complications after abdominoplasty.
Causes: Disruption of lymphatic channels during dissection, large tissue removal, or inadequate compression.
Prevention: Limited undermining of tissues, use of quilting sutures, drains, and compression garments.
Management: Minor seromas are treated conservatively with compression and rest. Larger seromas may require repeated sterile aspiration in the clinic. Persistent cases may be managed with ultrasound-guided drainage or reinsertion of a drain. In chronic cases, a pseudobursa (encapsulated fluid pocket) can form and may require surgical removal.
Wound Healing Problems and T-Junction Dehiscence

Wound breakdown
The T-junction, where the vertical and horizontal incisions meet, is under high tension and prone to delayed wound healing or wound breakdown.
Causes: Excess tension, poor blood supply, infection, or nutritional deficiency.
Prevention: Gentle tissue handling, tension-reducing sutures, and proper postoperative support garments.
Management: Minor separation is managed with local dressings and wound care. Moderate cases benefit from LED light therapy, topical wound-healing agents, or negative-pressure dressings. Persistent cases may require revision surgery or minor debridement to encourage closure.
Wound Infection
Wound infection occurs in approximately 2–6% of cases and typically appears within the first 10 days post-surgery. Signs include redness, warmth, swelling, pain, or discharge.
Causes: Bacterial contamination, poor hygiene, or reduced blood flow to the area.
Prevention: Strict sterile technique during surgery, prophylactic antibiotics, and proper wound hygiene at home.
Management: Superficial infections respond to oral antibiotics and wound cleaning. Deep infections or abscesses may need hospital admission, intravenous antibiotics, and drainage.
Bleeding and Haemorrhage
Bleeding can occur intraoperatively or postoperatively, particularly in patients on anticoagulant therapy or with uncontrolled hypertension.
Prevention: Careful blood pressure control and meticulous haemostasis during surgery.
Management: Minor bleeding may be treated conservatively with compression and observation. More significant bleeding requires return to the operating theatre for exploration. Tranexamic acid can be used to reduce blood loss and drain output (7).
Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
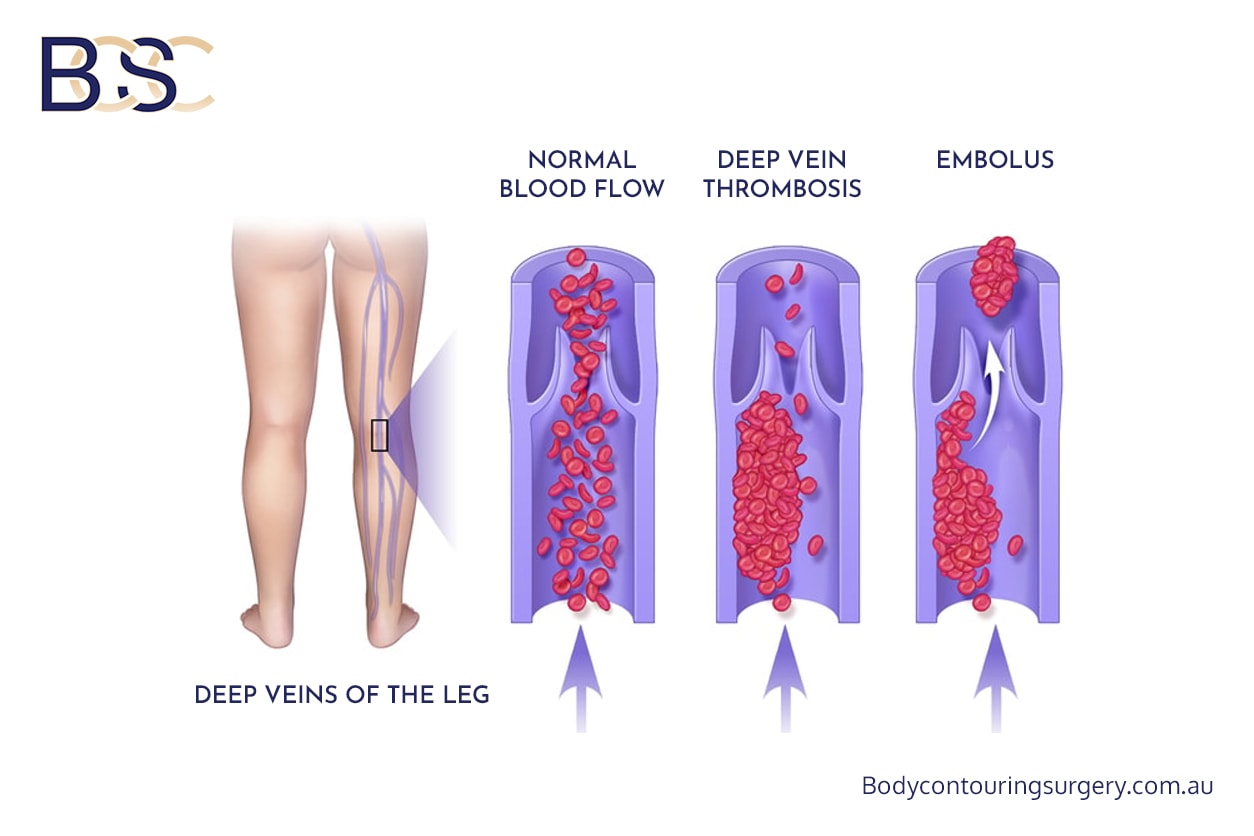
DVT and PE
These are rare but serious potential complications associated with prolonged immobility.
Prevention: Early mobilisation, calf compression devices, pharmacologic anticoagulation, and adequate hydration.
Management: Confirmed DVT is treated with anticoagulant therapy, monitoring for symptoms such as calf pain or swelling. Pulmonary embolism presents with shortness of breath or chest pain and requires urgent hospital management.
Hypertrophic Scars and Scar Widening
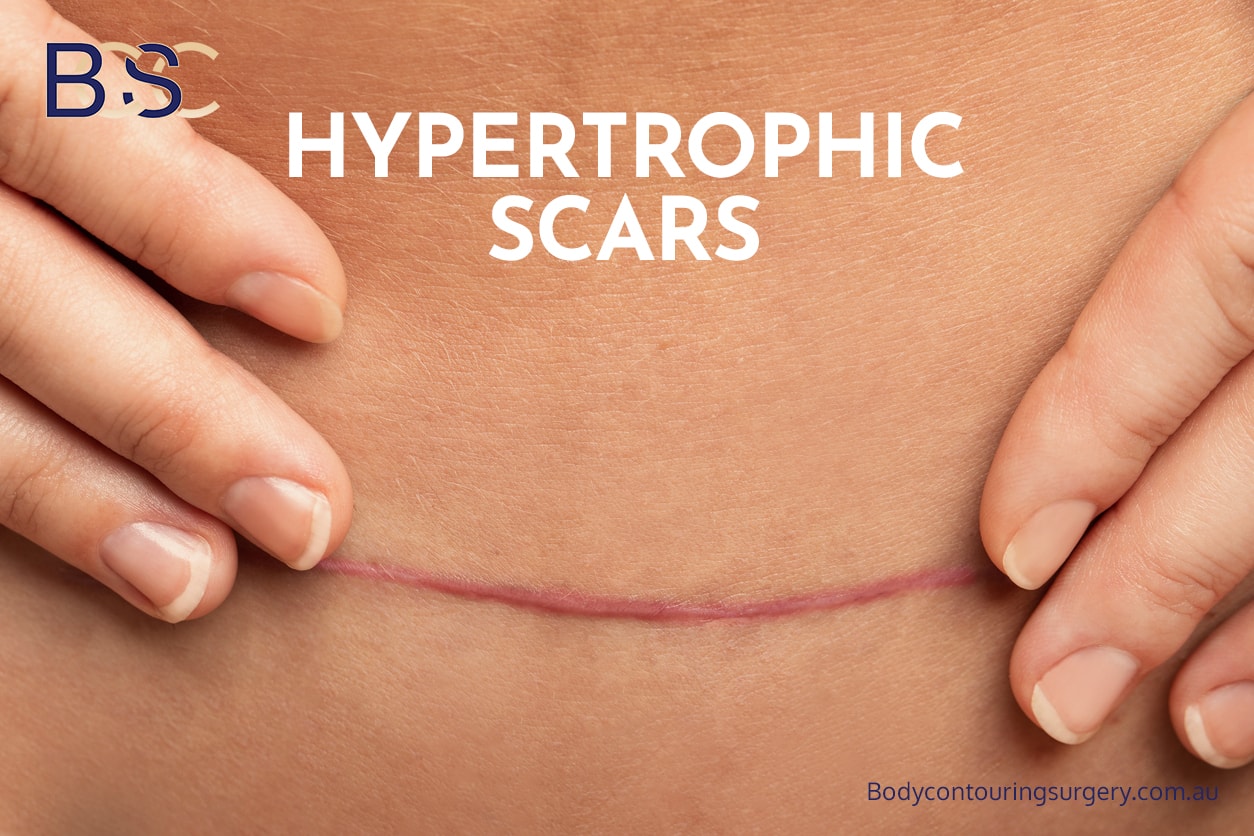
Hypertrophic scars
Scars may become thickened, raised, or stretched due to excessive tension during healing.
Prevention: Tension-free closure, scar taping, and silicone therapy.
Management: Silicone gels, scar massage, and laser therapy are common treatments. Persistent hypertrophic scars can be revised surgically after full maturation (usually after 12 months).
Nerve-Related Complications
During Fleur-de-Lis abdominoplasty, fine sensory nerves in the abdominal wall can be affected, leading to temporary numbness or altered sensation.
Presentation: Tingling, hypersensitivity, or numbness across the lower abdomen or upper thighs.
Prevention: Careful dissection techniques to preserve nerve pathways.
Management: Sensory changes occur over months as nerves regenerate. For persistent discomfort, desensitisation therapy, topical anaesthetic creams, or neuropathic pain medications may help. Rarely, long-term numbness can occur.
Liposuction (suction-assisted lipectomy) Related Issues
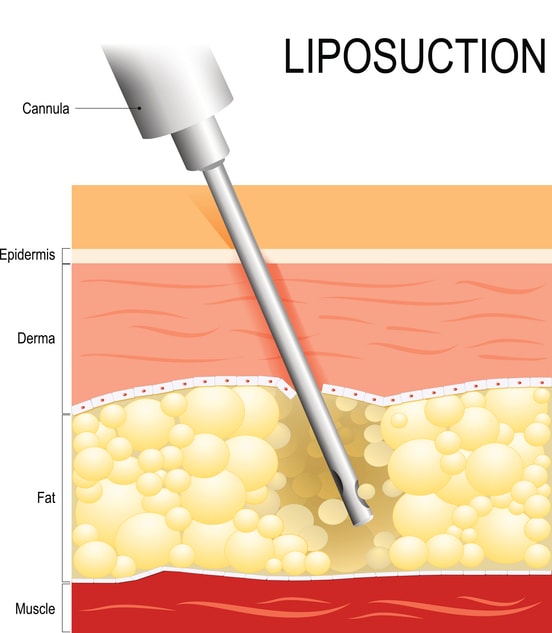
Liposuction
When liposuction (suction-assisted lipectomy) is performed alongside abdominoplasty, there is added potential for irregularities or skin discolouration.
Prevention: Gentle, uniform technique and avoiding over-aggressive fat removal.
Management: Mild contour irregularities are usually treated conservatively with no intervention and change over time. Lymphatic massage and skin tightening procedures may assist. In rare cases, a minor revision may be considered once healing stabilises.
Anaesthetic Complications

General anaesthetic
All major surgical procedures involve anaesthetic risks. Anaesthetic complications may include nausea, vomiting, sore throat, or temporary dizziness.
Prevention: Preoperative anaesthetic assessment identifies allergies and airway risks.
Management: Postoperative nausea is treated with antiemetic medication. Airway irritation typically resolves within a few days. Severe reactions, though uncommon, are promptly managed by the anaesthetic team in hospital.
Risk Factors Influencing Complication Rates
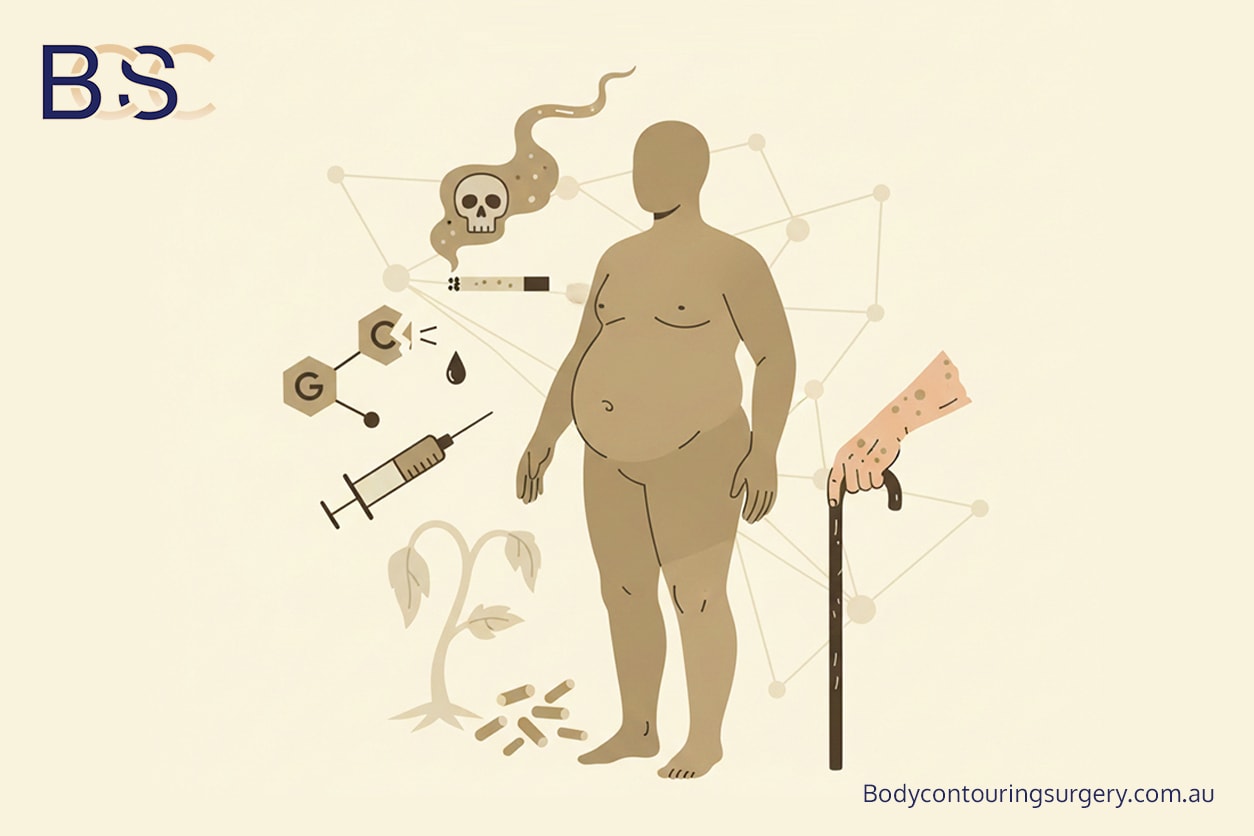
Common risk factors reported in Aesthetic Surg J and Plast Reconstr Surg include:
- High body mass index (BMI): Associated with wound tension and slower recovery. Obese patients are at increased risk for postoperative complications, such as wound healing problems and thromboembolic events, and require careful preoperative planning.
- Diabetes: Impairs microcirculation and increases wound healing time.
- Smoking: Restricts oxygen delivery to the surgical site.
- Nutritional deficiencies: Reduce collagen synthesis and delay tissue repair.
- Advanced age and resection weight: Correlate with longer recovery and increased risk of wound complications.
Understanding these risk factors is critical for outcomes and reducing the likelihood of major complications.
Supporting Healing and Complications
At BCSC, our Specialist General Surgeons (FRACS) focus on holistic preparation, precise surgical techniques, and structured postoperative care. A specialist surgeon plays a key role in assessing recovery, providing post-operative guidelines for post weight loss patients.

Surgical team
Strategies for Safer Recovery
- Preoperative optimisation: Managing chronic illness, achieving stable weight, and correcting deficiencies.
- Intraoperative care: Use of tension-reducing sutures and minimal undermining to preserve blood flow.
- Advanced wound care: Negative-pressure dressings such as PICO systems and LED light therapy for improved recovery.
- Postoperative support: Regular nurse follow-ups, wound reviews, and guidance on nutrition and mobilisation.
These evidence-based practices help minimise delayed wound healing, reduce seroma formation, and support recovery for patients after massive weight loss. Once healing is complete, many patients report functional benefits, including posture and skin comfort.
Comparative Complication Data

Comparative Complication Data
|
Complication Type |
Fleur-de-Lis (%) |
Traditional (%) |
Extended (%) |
|---|---|---|---|
|
Total Complications |
41.9 |
28.0 |
33.0 |
|
Major Complications |
5.0 |
3.0 |
4.0 |
|
Wound Healing Problems |
32 |
18 |
25 |
|
Seroma |
9.5 |
7.0 |
8.0 |
|
Bleeding |
10.8 |
6.0 |
7.5 |
|
Deep Vein Thrombosis |
0.5 |
0.3 |
0.4 |
(Data sourced from Aesthetic Surg J, Plast Reconstr Surg, Ann Plast Surg, and Br J Plast Surg, 2010–2025.)
Conclusion
The Fleur-de-Lis abdominoplasty remains an effective reconstructive surgery option for patients with significant weight loss and extensive excess skin. Although the operation carries higher complication rates than traditional abdominoplasty, most concerns are manageable with early intervention.
When performed by qualified Specialist General Surgeons (FRACS) in accredited hospitals, the procedure can help treat abdominal function, comfort, and hygiene for post bariatric patients. Each patient’s results are unique, and long-term success depends on good preparation, close follow-up, and realistic expectations.
- Parsa AA, McKnight CL, Macias LH, et al. Complications and risks associated with the different types of abdominoplasties. Plast Reconstr Surg Glob Open. 2024;12(3):e5001–e5009.
- Sommer B, Westphal F, Strauss B, et al. Post-bariatric abdominoplasty: analysis of 406 cases with focus on risk factors and complications. Aesthetic Surg J. 2021;41(5):NP450–NP462.
- Hester TR, Baird W, Nahai F, et al. Fleur-de-Lis abdominoplasty: a safe alternative to traditional abdominoplasty for the massive weight loss patient. Plast Reconstr Surg. 2010;125(1):45–55.
- Mistry RM, Tanna N, Morrison CM, et al. Fleur-de-Lys abdominal body contouring surgery following massive weight loss. J Plast Reconstr Aesthet Surg. 2021;74(3):613–620.
- Hurwitz DJ, Holland SW. The Fleur-de-Lis abdominoplasty. Aesthetic Surg J. 2014;34(3):432–443.
- Saad A, Almutairi K, Shakir S, et al. Complications following abdominoplasty in post-weight loss patients: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2025;78(1):11–22.
- Johnstone DJ, Parker ML, Zhen C, et al. Systemic tranexamic acid for reduced postoperative blood loss and less bleeding. Plast Reconstr Surg Glob Open. 2024;12(2):e4808–e4815.