Overview of Abdominoplasty After Weight Loss: Understanding Risks and Recovery
At the Body Contouring Surgery Clinic (BCSC), our team of specialist surgeons perform a wide range of body contouring surgery procedures for patients who have achieved massive weight loss. Many have lost a significant amount of body weight through bariatric surgery, gastric bypass surgery, or lifestyle changes. While achieving significant weight loss can have positive health effects, it may also result in excess skin, weakened abdominal muscles (diastasis recti), and changes in skin elasticity. These anatomical changes may lead some patients to consider abdominoplasty (tummy tuck).
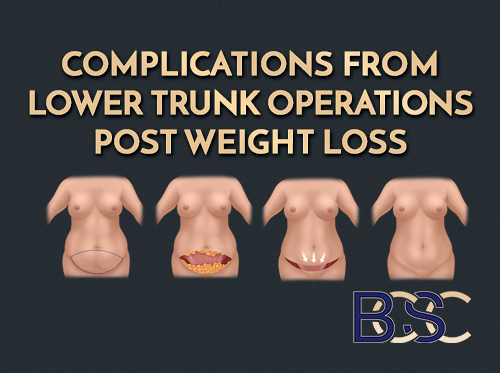
Understanding the potential abdominoplasty post weight loss complications is essential for patients and healthcare professionals. Both standard and extended abdominoplasty are major surgical procedures, and as with any operation, there are risks and possible postoperative complications. Research shows that complication rates after post bariatric abdominoplasty range from 18% to 53%, depending on individual risk factors, nutritional status, and surgical extent (Myszkowska 2025; Chaker 2024; Liao 2024).

Abdominoplasty complication rates
This review outlines findings from peer-reviewed research, including the Aesthetic Surgery Journal, to help patients understand potential surgical complications, prevention strategies, and the general recovery process. It should not be interpreted as medical advice or a guarantee of outcomes.
Understanding Abdominoplasty Surgery After Weight Loss
An abdominoplasty (tummy tuck) is a common body contouring procedure performed after massive weight loss. It aims to remove excess skin & repair separated abdominal muscles (diastasis recti). At BCSC, surgical plans are tailored to each patient’s anatomy, weight loss history, and medical needs.
Patients may undergo:
Standard abdominoplasty
Removes excess skin and adipose tissue in the lower abdomen.
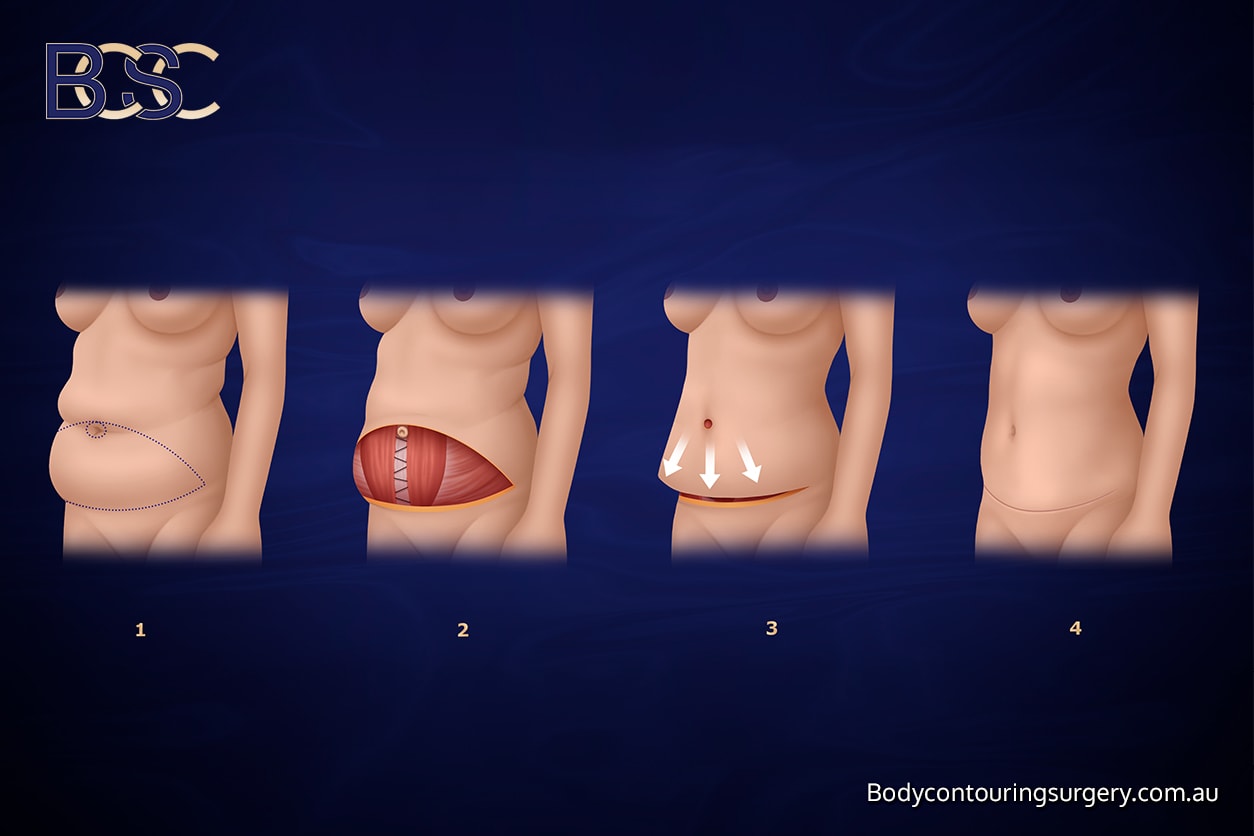
Full abdominoplasty
Extended abdominoplasty
Extends around the flanks to remove excess skin from the sides and abdomen.
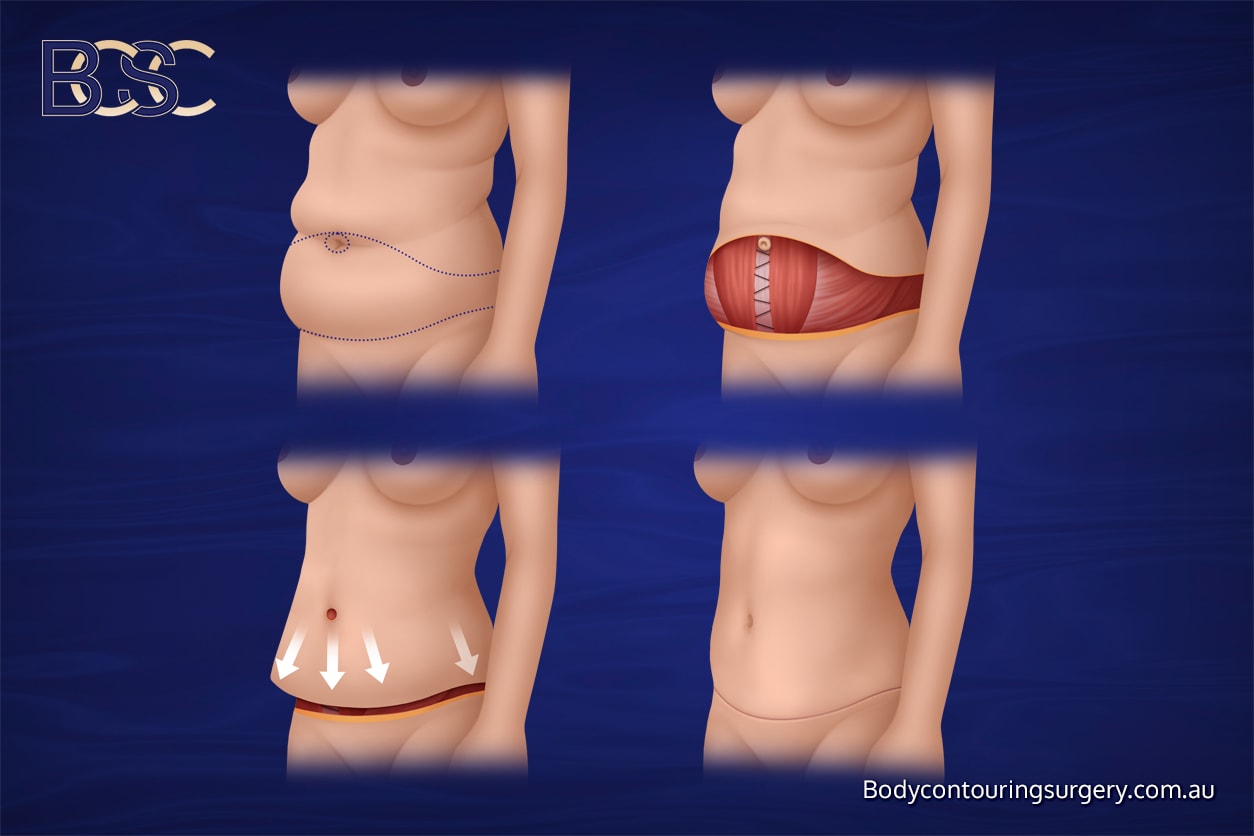
Extended abdominoplasty
Fleur-de-lis abdominoplasty
Removes excess skin both vertically and horizontally for patients with significant midline laxity.
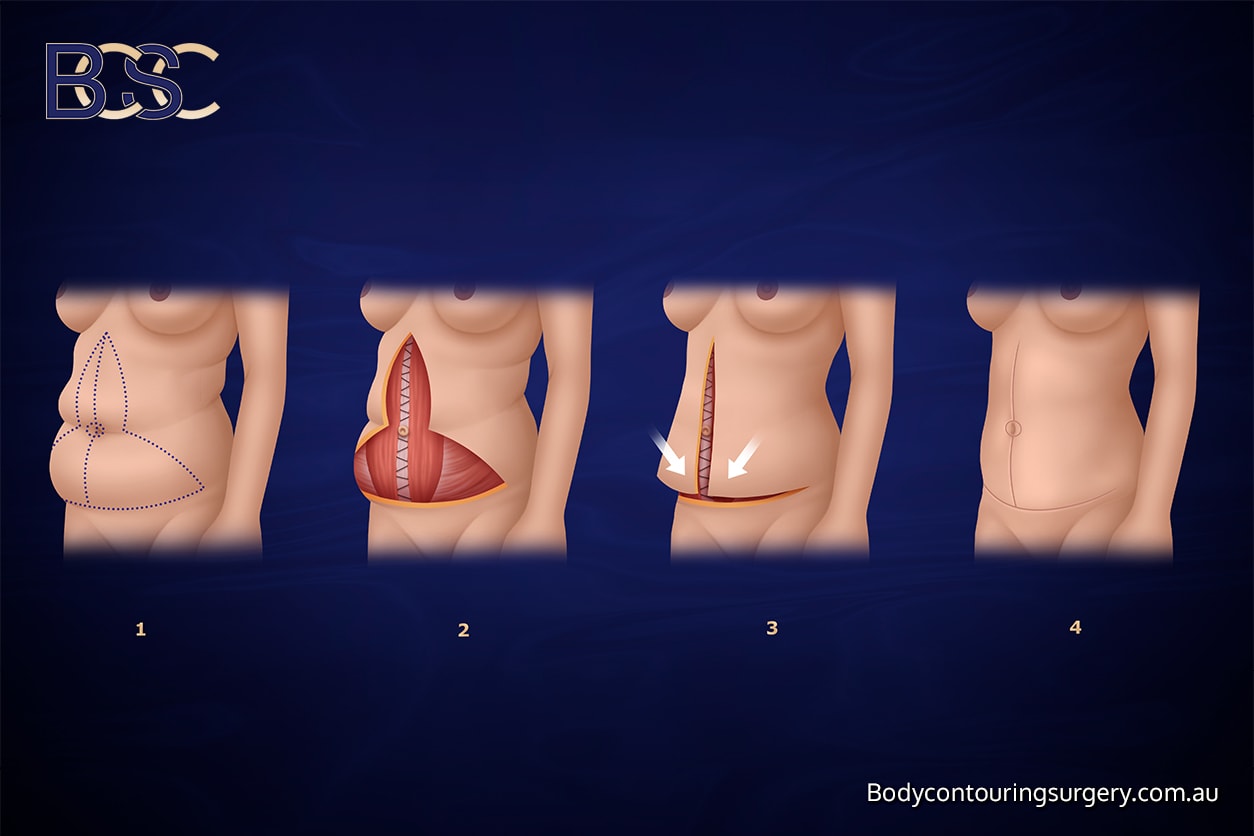
Fleur-de-lis abdominoplasty
Abdominal lipectomy or apronectomy
Removes an overhanging apron of skin (pannus), often seen in post bariatric surgery patients.
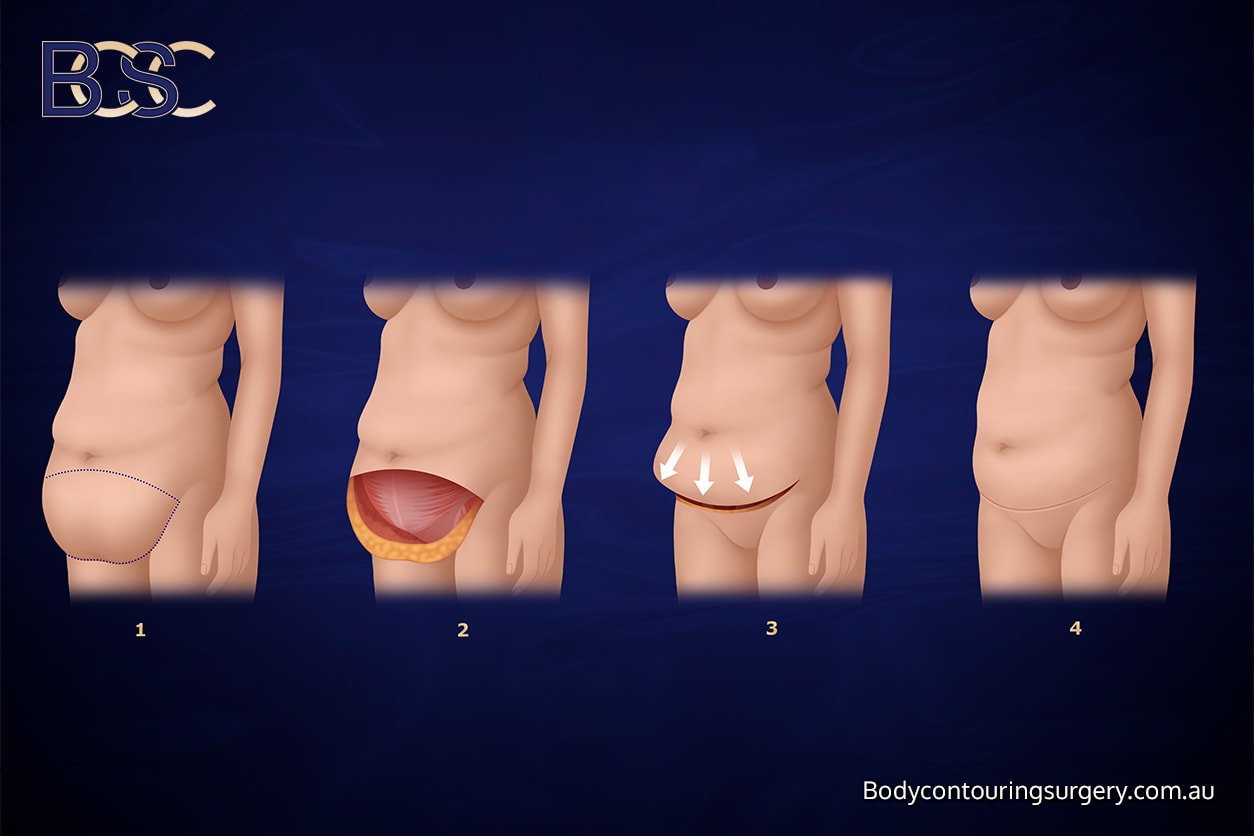
Abdominal lipectomy or apronectomy
For patients:
These abdominal contouring operations are complex and require careful risk factor analysis, preoperative assessment, and multidisciplinary planning. Individual results vary.
Why Complications Are More Common After Major Weight Loss
Post bariatric patients and individuals who have undergone weight loss surgery such as gastric bypass or laparoscopic gastric banding may have unique anatomical and metabolic factors that affect healing. The combination of excess skin, reduced circulation, and nutritional challenges increases the likelihood of both minor and major complications.

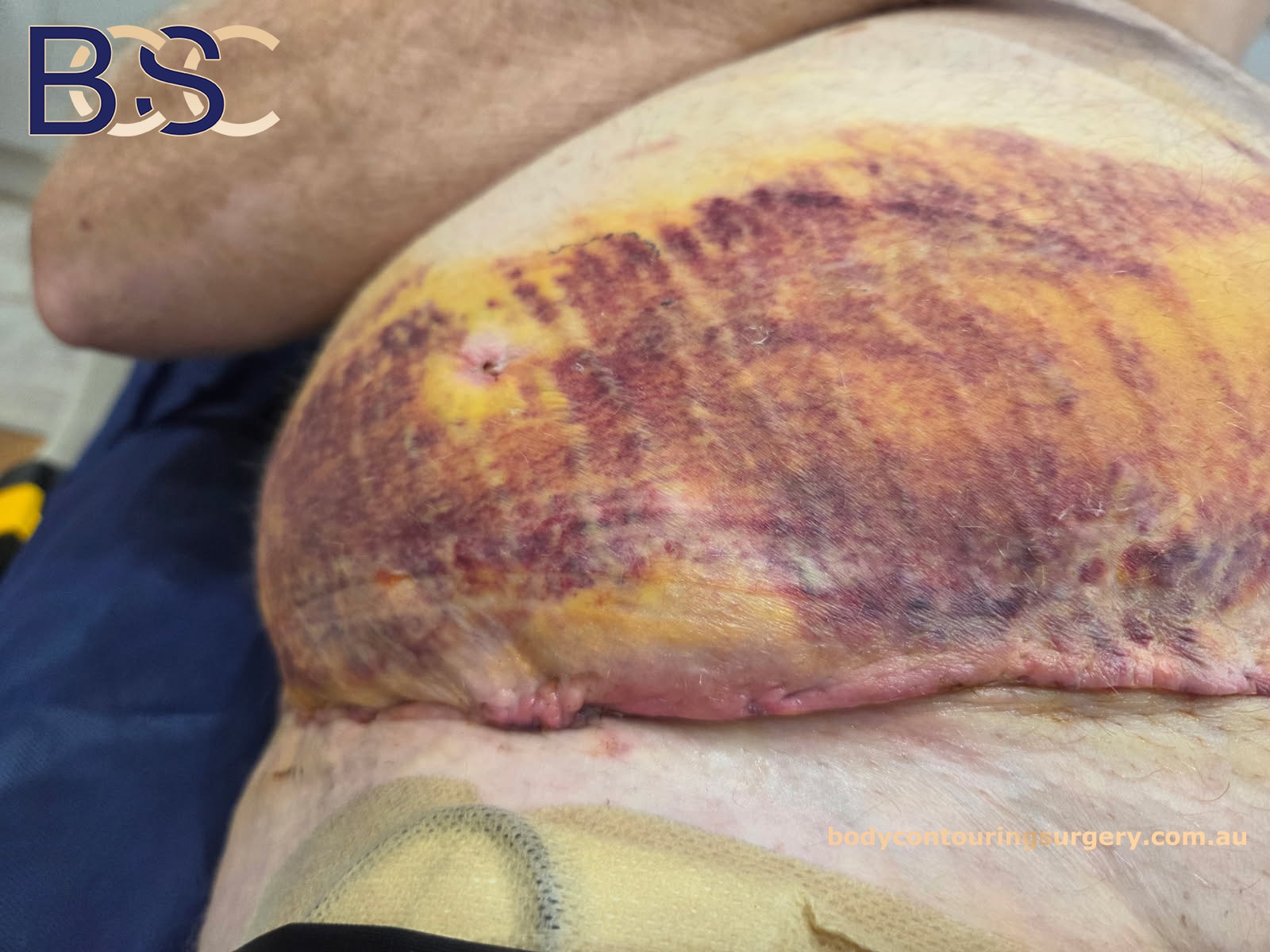
Wound breakdown treated by VAC dressing
Key risk factors include:
- Reduced skin elasticity and circulation: Long-term obesity can stretch tissues, reducing blood flow.
- Nutritional deficiencies: Common in bariatric surgery patients due to decreased nutrient absorption.
- Elevated BMI or ongoing excess weight: Adds tension to surgical sites and can delay healing.
- Comorbidities: Conditions such as diabetes, anaemia, or vascular disease may affect wound healing.
- Smoking or inactivity: Impairs oxygenation and increases wound complications.
Myszkowska et al. (2025) found that post bariatric abdominoplasty patients have higher complication rates compared to typical cosmetic cases due to these factors.
For patients:
Reaching a stable weight and correcting nutritional deficiencies before surgery may help reduce the likelihood of postoperative complications.
Common Abdominoplasty Complications After Weight Loss
Wound Healing Concerns and Seroma Formation

Deep wound infection
A seroma (fluid collection under the skin) is one of the most common post weight loss complications following abdominoplasty. Research indicates that using progressive-tension sutures and preserving Scarpa’s fascia can reduce this risk (Liao 2024).
Wound infections occur in approximately 1–4% of post bariatric patients, while wound separation (dehiscence) can occur in up to 10–15% of cases. Most of these are managed with dressings, antibiotics, or negative pressure therapy.
For patients:
Minor wound issues are relatively common in specialist surgery and are usually treatable with medical management and follow-up.
Haematoma and Postoperative Bleeding
haematoma post surgery
Haematoma, or internal bleeding beneath the skin, can occur in approximately 2–7% of patients. It is often associated with increased risk from hypertension or anticoagulant use. Experienced specialist surgeons reduce this risk through meticulous surgical technique and haemostasis.
The outcomes analysis by Chaker et al. (2024) reported that major complications requiring hospitalisation occurred in 2.1% of patients undergoing abdominoplasty.
For patients:
Prompt communication with the surgical team is important if unexpected swelling or pain develops post-surgery.
Scarring and Skin Changes

wound breakdown post surgery
All reconstructive surgery results in some form of scarring, and abdominoplasty (tummy tuck) is no exception. The pattern, length, and final appearance of scars depend on factors such as incision placement, individual healing response, skin elasticity, and surgical technique. Following massive weight loss, many patients express concern about visible scars, as the procedure often requires long incisions to effectively remove excess skin and re-drape tissue.
Scars from a standard abdominoplasty usually extend from hip to hip, positioned low enough to be covered by most underwear or swimwear. In an extended abdominoplasty, the incision continues around the sides to treat laxity of the flanks. For some post bariatric surgery patients, a fleur-de-lis abdominoplasty may also be used, which adds a vertical midline scar to treat upper and lower abdominal skin redundancy.
In the early healing phase, scars can appear red, raised, or firm. Over several months, they typically flatten and fade, becoming lighter in colour. The process of scar maturation can take up to 12–18 months. During this time, the body continues to remodel collagen within the scar tissue, and the appearance gradually softens and fades over time. Patients with darker or olive-toned skin may be more prone to hyperpigmented or hypertrophic scars, while individuals with very fair skin may notice redness lasting longer.

Distribution of complications for abdominoplasty post surgery
Several factors can influence how scars heal, including genetics, nutritional status, infection, or tension along the incision line. Poor wound healing due to nutritional deficiency or smoking may cause widened scars or areas of wound separation. To support the functional results, specialist surgeons often use layered closure techniques and tension-reducing sutures to distribute stress evenly along the incision.
Scar management begins soon after the wound has fully closed. Common methods include silicone gel sheeting or topical silicone gels, gentle scar massage, and sun protection to prevent darkening of the scar line. In selected cases, laser therapy, microneedling, or reconstructive revision surgery may be considered to refine the scar appearance. However, these are generally secondary procedures performed months or years after initial healing.
For patients:
It is important to remember that all abdominoplasty surgeries result in some visible scarring, which is a normal and expected part of the healing process. Following postoperative care guidelines, avoiding smoking, maintaining a stable weight, and protecting scars from sun exposure all contribute to long-term outcomes. Regular follow-up appointments allow your surgical team to monitor healing and provide guidance on scar management throughout your recovery.
Nerve-Related and Sensory Changes
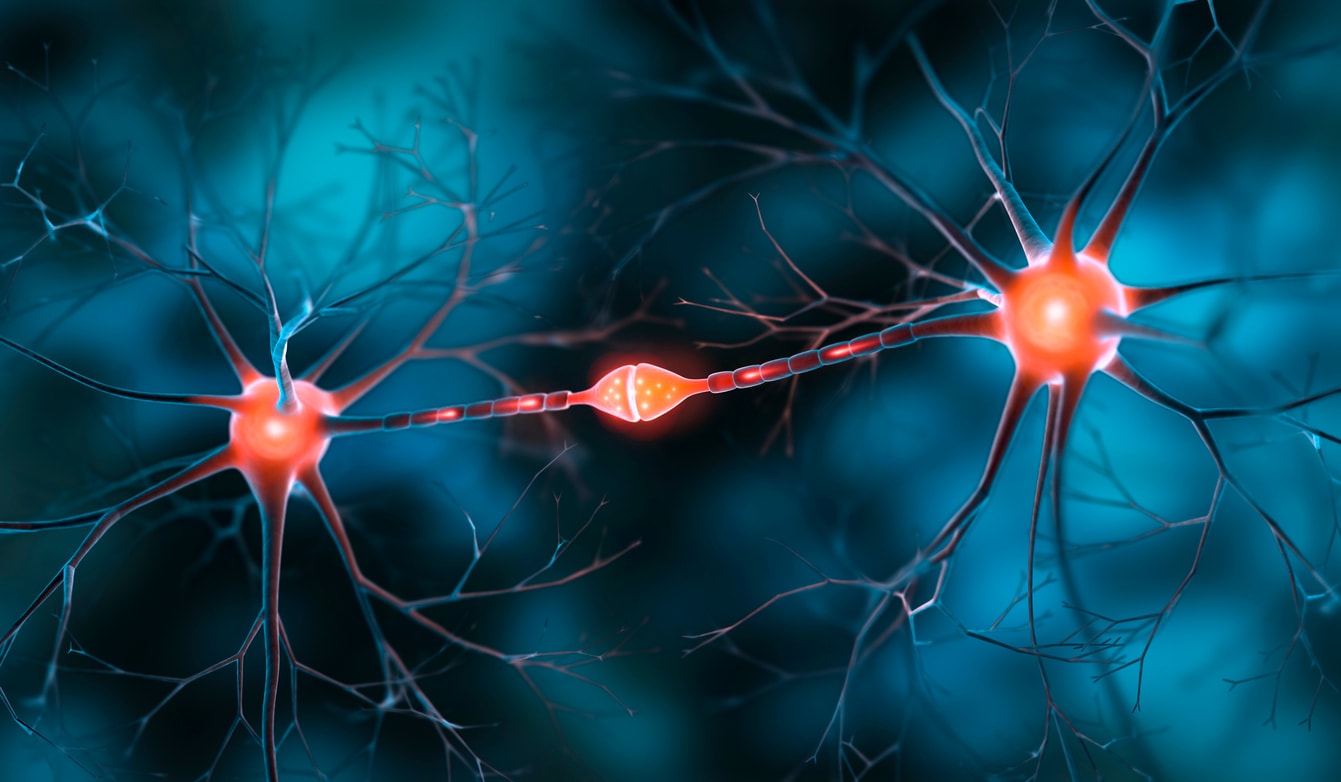
Nerve-Related and Sensory Changes
During abdominoplasty (tummy tuck), small sensory nerves beneath the skin of the lower abdomen are sometimes disrupted as excess tissue is lifted and repositioned. This can lead to temporary numbness, tingling, or reduced sensitivity in the lower abdominal area, the pubic region, or occasionally near the upper thigh. These sensations are a common part of recovery and usually change as the body heals. Most patients notice a gradual return of sensation within three to six months, but full recovery can take longer in some cases.
For some post-bariatric patients, these sensory changes may feel unusual or cause anxiety. It is important to understand that temporary nerve effects are not usually a sign of nerve damage, but rather a normal response to tissue repositioning and swelling. In rare situations, small branches of sensory nerves may become irritated or trapped in scar tissue, which can result in localised sharp or burning sensations known as nerve-related discomfort. These typically lessen over time as the nerves adapt.
In a few cases, patients experience heightened sensitivity or areas of tingling as nerve regeneration occurs. These symptoms may appear weeks or months after surgery as nerve fibres reconnect. Treatment options include non-invasive management options such as gentle massage, desensitisation techniques, and nerve-soothing medications. Physiotherapy can also be beneficial in retraining sensation during the healing process.
Specialist surgeons take steps to protect as many nerve branches as possible during surgery by maintaining careful dissection planes and minimising tension on the tissues. Preserving the integrity of deeper nerve pathways helps reduce the extent of postoperative numbness and supports recovery.
For patients:
Experiencing some numbness, tightness, or altered skin sensation after abdominoplasty surgery is expected and typically temporary. These changes should steadily normalise, although recovery times vary widely. If persistent or painful nerve sensations occur, these can often be managed effectively through medical review and supportive care.
Less Common Complications
- Skin or Umbilical Necrosis: A rare issue, seen in fewer than 3% of patients, often linked to reduced blood flow or smoking.
- Fat Necrosis: Occurs when small areas of fat lose blood supply, leading to firm nodules that usually resolve naturally.
- Wound Dehiscence: Partial wound separation can occur in 3–10% of post bariatric surgery patients. Managed with dressings or, rarely, minor surgical repair.
For patients:
Maintaining good nutrition and avoiding smoking can assist the healing process.
Serious and Rare Complications
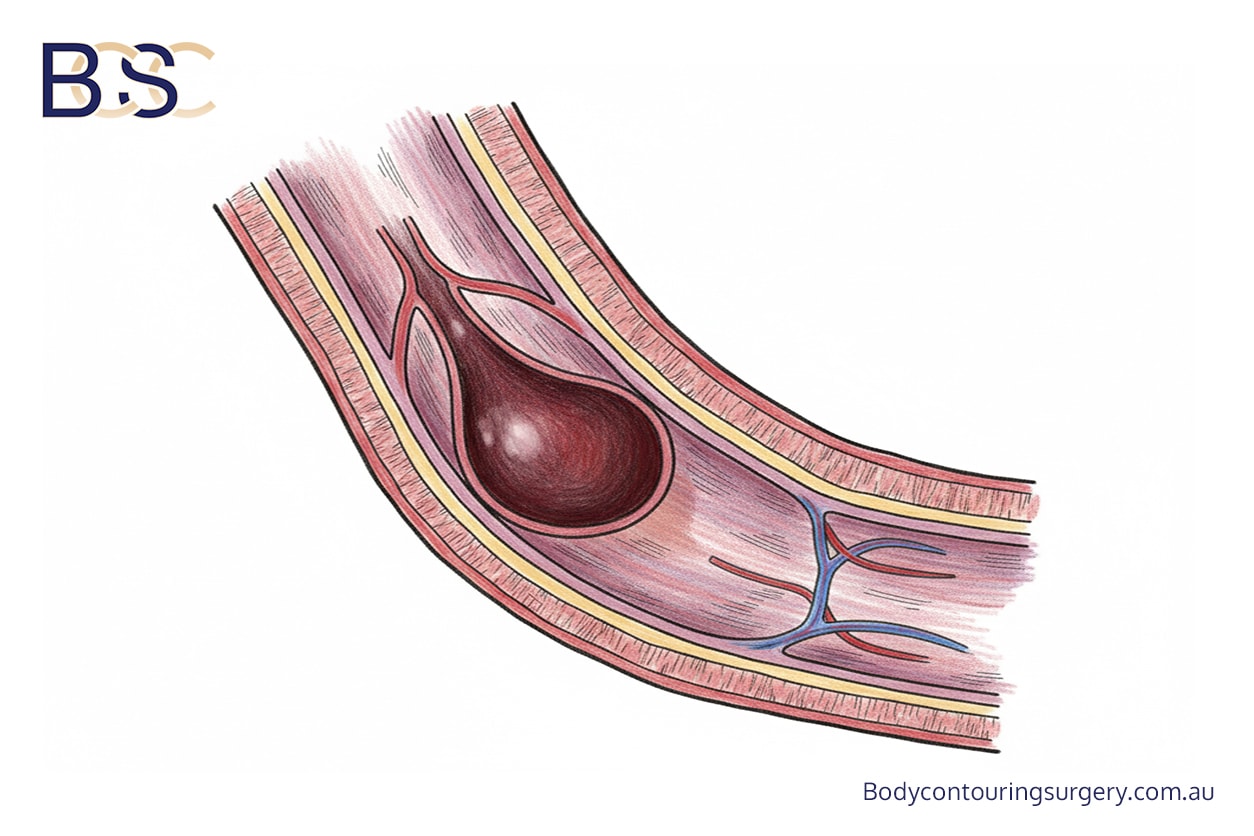
Deep vein thrombosis
- Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE): Rare but serious events (0.5–2% incidence). Preventative steps include early ambulation, compression garments, and anticoagulant use where appropriate.
- Major Bleeding: Occurs in about 1% of cases and may require return to theatre.
- Anaesthetic Complications: These are uncommon (<1%) and are carefully screened for by anaesthetists prior to surgery.
For patients:
Procedures are conducted in accredited hospitals under FRACS-qualified specialist surgeons following strict safety protocols.
Reducing Risk and Supporting Recovery

Reducing Risk and Supporting Recovery
|
Risk Factor |
Impact on Surgical Outcomes |
|---|---|
|
BMI ≥30 kg/m² |
Increases risk of wound and seroma formation |
|
Smoking |
Impairs oxygenation and delays wound healing |
|
Diabetes / Malnutrition |
Increases infection risk |
|
Large tissue removal |
Raises risk of bleeding and seroma formation |
|
Prolonged surgery |
May increase risk of infection or deep vein thrombosis |
For patients:
Maintaining a stable weight, and following medical advice before and after surgery can help recovery.
Prevention and Postoperative Care
Preventing postoperative complications involves shared responsibility between the patient and the surgical team. Evidence-based strategies include:
- Optimising nutritional and medical conditions before surgery.
- Planning surgical incisions to preserve blood supply.
- Using drains or tension-reducing sutures where appropriate.
- Wearing compression garments to reduce swelling.
- Mobilising early after surgery to reduce the risk of blood clots.
- Attending follow-up reviews for early detection of any concerns.
For patients:
Adhering to medical guidance and maintaining follow-up care supports healing and more predictable outcomes.
Frequently Asked Questions

What should I know before having abdominoplasty?
Patients should understand the recovery timeline, possible scarring, and the potential for complications. Recovery experiences differ from person to person.
What is the most common complication after abdominoplasty?
The most common issues include seroma formation, wound infections, and wound separation. These are typically mild and managed with conservative care.
Who may not be suitable for abdominoplasty?
Those with unstable medical conditions, ongoing excess weight, or nutritional deficiencies may not be suitable until optimised.
What happens if further weight loss occurs after surgery?
Additional weight loss can lead to excess skin recurrence. It is preferable to achieve a stable weight for several months before surgery.
How long is recovery after abdominoplasty?
Recovery timelines vary. Some individuals may resume light activities after several weeks, while full recovery may take months.
Conclusion
Abdominoplasty after weight loss can remove excess skin, though outcomes vary between individuals. Like all reconstructive surgeries, it carries potential surgical complications and requires careful preparation. At BCSC, body contouring surgery is performed by specialist surgeons in accredited hospitals to ensure adherence to quality standards.
- Myszkowska B, Zawada-Wiśniewska P, Handzlik I, Krakowiak M. Complications following abdominoplasty in post-weight loss patients: a systematic review and meta-analysis. South Asian Res J Bus Manag. 2025;7(5):413–9.
- Cannizzaro Hospital Group. Experience in post-bariatric abdominoplasty for patients with significant weight loss: a prospective study. J Pers Med. 2024;14(7):681.
- Chaker SC, Hung YC, Saad M, Perdikis G, Grotting JC, Higdon KK. Complications and risks associated with different types of abdominoplasties: an analysis of 55,596 patients. Aesthet Surg J. 2024;44(9):965–75.
- Liao CD, Zhao K, Nikkhahmanesh N, Bui DT. Decreasing seroma incidence following abdominoplasty: a systematic review and meta-analysis of high-quality evidence. Aesthet Surg J Open Forum. 2024;6:o-jae016.
- Sadeghi P, Duarte-Bateman D, Ma W, Khalaf R, Fodor R, Pieretti G, et al. Post-bariatric plastic surgery: abdominoplasty, the state of the art in body contouring. J Clin Med. 2022;11(15):4315.
- Stein MJ, Karaev S, Matarasso A. A primer on abdominoplasty safety. Plast Surg (Oakv). 2024;32:e1–14.
- Winocour JN, Grotting JC, Higdon KK. The safety profile of abdominoplasty: analysis of 25,478 cases from the CosmetAssure database. Plast Surg (Oakv). 2024;32:e1–14.
- Matarasso A, Wallach SG, Rankin M, Galiano RD, Zienowicz R. Abdominoplasty survey: current practices and complications. Plast Reconstr Surg. 2006;117(6):1797–808.