Preventing, Diagnosing, and Managing Nerve Injury After Brachioplasty Surgery
Brachioplasty, when conducted by experienced practitioners, is associated with predictable outcomes and manageable risks, although, though rare, nerve injury is possible. The most common nerve injury affects the medial antebrachial cutaneous nerve since it is found within the dissection plane. Nerve damage during brachioplasty can cause pain, chronic numbness, or decreased mobility, which may be lasting unless promptly treated. Non-surgical or surgical interventions may alleviate these symptoms.
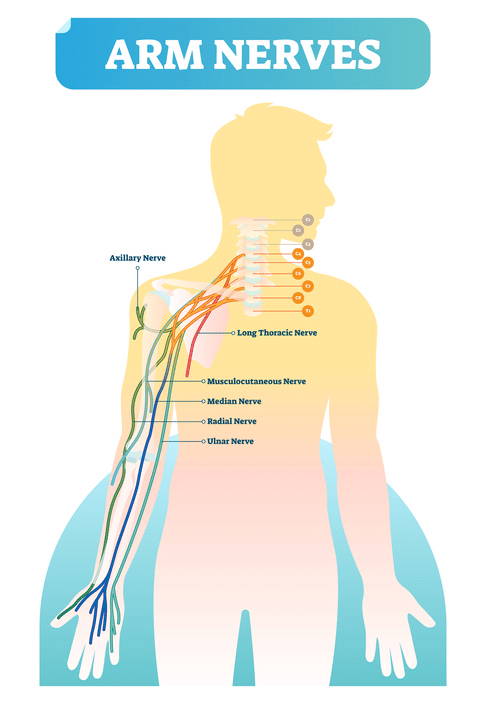
What major nerves are in the arm?
The brachial plexus consists of nerves affecting skin sensation and muscle movements within the hand, arm, and shoulder. The nerve roots begin at the spinal cord and run down the entire length of the arm. The brachial plexus nerves include the:
- Ulnar nerve
- Radial nerve
- Axillary nerve
- Median nerve
- Musculocutaneous nerve
Arm Nerve Injuries After Brachioplasty
- Medial brachial cutaneous nerve injury is the most common brachial plexus injury that occurs during brachioplasty, affecting an estimated five in 100 patients. (Ref 1)
- Neuroma is a painful condition in which a bundle of benign nerve tissue becomes trapped in the scar tissue as the nerves heal from surgery.
- The ulnar nerve, radial nerve, and median nerve can become compressed from excessive swelling in the arms post-surgery.
What happens when the arm nerves are damaged?
Medial brachial cutaneous nerve injury and other types of nerve damage may cause sensation changes, pain, swelling, paralysis, or restricted movement.
Nerve Injury Symptoms
An injured nerve in the arm can lead to one or more of the following:
- Edema
- Muscle weakness
- Tingling or numbness
- Neuropathic pain ranging from mild to severe
- Motor impairment due to loss of nerve function
- Compartment syndrome (swelling, tenderness, and pink skin)
Is nerve pain, numbness, or tingling normal after Brachioplasty surgery?
Immediately after brachioplasty, the arms and hands can have significant swelling and firmness. Pain and tenderness are also a normal part of the healing process, which can temporarily decrease your range of motion. Numbness and shooting nerve pain are also common as the superficial nerves heal over the next three months. These symptoms are rarely a cause for alarm.
“An important part of the Brachioplasty consultation is letting your patient know what to expect after surgery,” Dr Bernard Beldholm explains. “Doing so will help them understand what is normal and what is not. A good surgeon will always see the patient for multiple follow-up appointments in the days and weeks after Brachioplasty surgery to make sure they are healing as expected. During these follow-up appointments, we can monitor for complications and manage them if any issues arise.”
When should a Brachioplasty patient worry about nerve pain or numbness?
Any unusual, severe, or worsening symptoms should be reported to your surgeon immediately. Your surgeon can provide follow-up care or refer you to a specialist for diagnostic tests and treatment if there is evidence suggesting a traumatic nerve injury, including damage to any of the brachial plexus nerves.
What diagnostic tests show nerve damage?
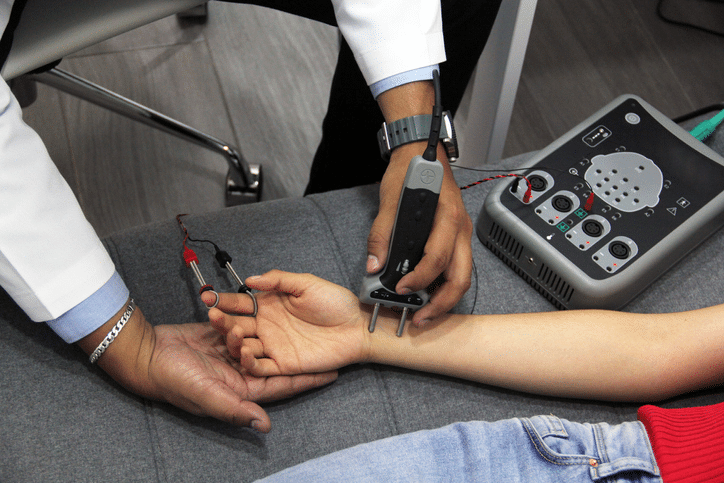
In addition to a visual or physical exam, there are several ways to diagnose nerve injuries.
Nerve conduction studies: A nerve conduction velocity (NCV) test measures nerve function by assessing how quickly an electrical impulse moves through a nerve. During a nerve conduction study, electrodes are placed on the skin to stimulate the nerve. Next, the speed of the electrical impulse is measured. Any abnormalities suggest nerve damage.
Electromyogram studies: Nerve cells called motor neurons communicate with the muscle to facilitate everyday movements. An EMG measures the electrical activity within the muscles, both while the affected muscle is contracted and resting. Sudden muscle weakness or immobility may be indicative of nerve damage.
Diagnostic imaging: High-resolution ultrasound and other imaging scans can accurately map out the sensory nerves within the arm to determine the site of an injured nerve. (Ref 2)
Exploratory surgery: If there is suspected nerve damage after Brachioplasty surgery, a surgeon may perform exploratory surgery to determine if one of the arm nerves has been injured or compressed. This is the most invasive option and carries more risks than nerve studies and diagnostic imaging exams.
Nerve Damage After Brachioplasty Surgery: What treatment options exist?
Mild paresthesia (tingling or numbness) after Brachioplasty surgery may resolve spontaneously, but not always. It is important to speak to your surgeon, especially if your symptoms are severe or gradually worsening. If they determine there is a nerve injury, the appropriate treatment depends on the type of nerve damage incurred. Options for managing a brachioplasty-related nerve injury may include the following:
Nerve blocks
Nerve blocks (also called neural blockades) relieve pain for up to 18 hours for acute nerve pain management.
Steroid injections
Injured nerves are slow to heal, but the process can be made with injectable steroids. These local injections may ease neuropathic pain, offering some relief as the nerve injury heals.
Analgesic Medications
Over-the-counter or prescribed pain relievers can reduce nerve pain as a damaged or injured nerve heals.
Surgical Release of the Skin Incision
Releasing the Brachioplasty skin incision is one of the most effective surgical interventions for moderate symptoms related to an arm nerve injury. (Ref 6)
Surgical Decompression of the Nerve
If a compression injury is suspected after Brachioplasty surgery, the surgeon may perform a skin incision release and also surgically decompress the nerve. (Ref 6)
Nerve Repair Surgery
If a section of the nerve is damaged, a surgical treatment may be performed to remove the injured segment and reconnect the healthy nerve ends together.
Nerve Grafting Surgery
A nerve graft is a type of reconstructive surgery that treats a gap or missing piece of nerve. This procedure is also known as a nerve transplant. It involves taking a piece of a healthy nerve and grafting it to fill the area where a nerve is partially missing. The grafted nerve may come from a cadaver (nerve allografting) or may be taken from the patient’s own body (nerve autographing). (Ref 5)
Physical Therapy
Physical therapy may help patients regain motor function, strength, and coordination after nerve injuries.
Shockwave Therapy
Low-energy extracorporeal shockwave therapy may potentially facilitate nerve healing and reduce inflammation around the nerve. This non-surgical procedure administers high-energy sonic pulses to the injured area and has shown promising effects on axon regeneration. (Ref 3)
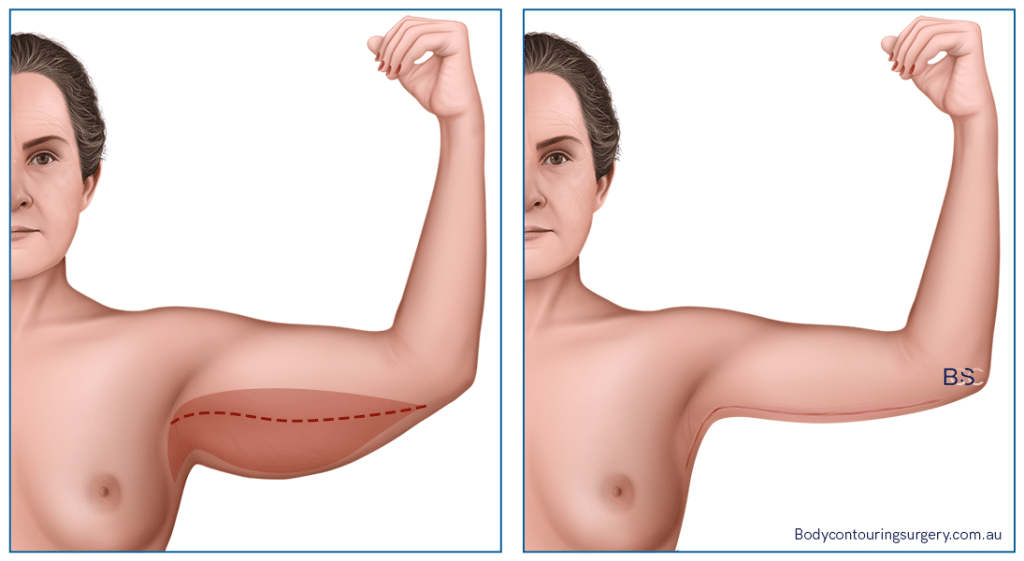
How can surgeons avoid nerve damage during Brachioplasty surgery?
Nerve injuries happen anytime a surgeon cuts into the skin. The superficial nerves typically heal over the next few months. However, major nerve damage can occur if the surgeon damages one of the major nerves in the arm.
The most commonly reported nerve injury from brachioplasty is medial brachial cutaneous nerve damage. (Ref 4) While rare, an estimated five percent of brachioplasty patients end up with this complication. (Ref 1)
Surgeons can decrease the risk of damaging this nerve by placing the brachioplasty incision closer to the back of the upper arms, rather than on the inner upper arm.
Regardless of the surgical scar placement, the surgeon must have extensive knowledge of the upper arm anatomy. This will help them avoid damaging major nerves or injuring other anatomical structures while they remove the excess skin and fat.
The surgeon must also be careful when they elevate the skin flap and perform the dissection. The upper arm skin lies close to the ulnar nerve and the terminal points of the medial brachial cutaneous (MBCN) and medial antebrachial cutaneous (MACN) nerves. (Ref 1)
Permanent Nerve Injury is Rare After Brachioplasty Surgery
Chronic nerve damage is extremely rare after brachioplasty. However, it is possible if the surgeon damages an otherwise healthy nerve during the operation.
References
- Chowdhry, Saeed. “Avoiding the Medial Brachial Cutaneous Nerve in Brachioplasty: An Anatomical Study.”PubMed Central (PMC), 2010.
- High-resolution Ultrasound as an Aid in the Diagnosis and Treatment of Post-brachioplasty Injury to the Medial Brachial and the Medial Antebrachial Nerves – Two Case Reports.” International Journal of Surgery Case Reports, vol. 72, Elsevier BV, Jan. 2020, pp. 520–23.
- Hausner, T., and Antal Nógrádi. “The Use of Shock Waves in Peripheral Nerve Regeneration.” International Review of Neurobiology, 2013, pp. 85–98.
- Knoetgen, James, and Steven L. Moran. “Long-Term Outcomes and Complications Associated With Brachioplasty: A Retrospective Review and Cadaveric Study.” Plastic and Reconstructive Surgery, vol. 117, no. 7, Lippincott Williams and Wilkins, June 2006, pp. 2219–23.
- “Nerve Graft (Nerve Transplant Surgery).” Johns Hopkins Medicine, 12 Dec. 2022.
- Al-Qattan, Mohammad M. “Multiple (Median, Ulnar, Radial and Medial Antebrachial) Nerve Injury Associated With Brachioplasty.” Journal of Hand and Microsurgery, vol. 12, no. S 01, Georg Thieme Verlag, Aug. 2020, pp. S78–80.