Compartment Syndrome After Brachioplasty Surgery
Acute compartment syndrome is a rare but serious condition that can occur after brachioplasty. Symptoms include severe pain, weakness, pale skin, and an inability to move the affected arm. If you suspect you have compartment syndrome after a surgical procedure such as an upper arm lift, seek immediate medical attention.
What is compartment syndrome?
Compartment syndrome is a serious condition caused by excess pressure building up within a muscle compartment. When pressure builds (for example, due to swelling from surgery or a traumatic injury) it can restrict blood flow and cause the muscle, nerves, or blood vessels to die. Compartment syndrome is typically isolated to one area of the body. It usually affects the forearm or lower leg. The hands, feet, buttocks, thighs, and upper arms can also develop compartment syndrome, although it’s less common in these areas.
Acute Compartment Syndrome vs Exertional Compartment Syndrome
There are two types of compartment syndrome. Acute compartment syndrome is the more serious of the two types. This is the type arm lift patients need to watch out for.
Acute Compartment Syndrome
Acute compartment syndrome tends to result from either a crush injury or surgery gone wrong. Symptoms often develop ** and immediate treatment is required. Acute arm compartment syndrome can be the result of arm lift (brachioplasty) surgery, although it is not a frequent complication.
Exertional Compartment Syndrome
Exertional compartment syndrome is usually gradual, temporary, and caused by repetitive physical activity. Typically, the pressure within the affected compartment flares up only during the activity, often resolving once the activity stops. Exertional compartment syndrome is less serious than acute compartment syndrome. It usually does not permanently affect limb function or mobility. However, the pain can be **. People affected by it may not be able to exercise or play sports as often as they would like.
What causes acute compartment syndrome in the arm?

Fascia (thin connective tissues) separate the muscle groups in the arms. Each layer of fascia has a confined space within it, called a compartment. The compartment contains nerves, muscle fibers, and blood vessels. If the compartment swells, it can lead to life-threatening issues for the patient.
Since the fascia can’t expand, any swelling within the compartment puts pressure on the fascia. As the pressure builds up, the blood vessels, muscles, and nerves become constricted. This is called acute compartment syndrome – a painful condition that can cause permanent injury if left untreated.
Top Causes of Acute Forearm Compartment Syndrome
- Arm surgery or crush injuries
- Severely bruised arm muscles
- Broken arm bones or severe sprains
- An arm cast, bandage, or tourniquet that is too tight
- Loss of blood supply in the arms due to positioning during surgery
Can an arm lift cause compartment syndrome?
While extremely rare, arm lift procedures can be a cause of compartment syndrome. The surgical technique matters. For example, if a surgeon removes too much loose skin and must forcefully close the incision, it can constrict the compartment. Likewise, if the surgeon takes too long to perform surgery, the arm can swell to the point that it’s difficult to close the incision. If the surgeon must force the wound closed, the patient might develop acute compartment syndrome.
Unfortunately, surgeons cannot always predict how much a patient will swell during surgery. Everybody is different. It’s possible to end up with compartment syndrome after an arm lift, even if your surgeon did everything right.
How common is compartment syndrome after an arm lift procedure?
Acute compartment syndrome is a rare outcome of arm lift surgery (brachioplasty). Most patients do not experience major complications such as this, but it can happen nevertheless. Be sure to choose a highly experienced specialist surgeon if you are considering an arm lift.
Compartment Syndrome Symptoms
Symptoms of acute compartment syndrome after upper arm surgery include:
- Pale skin in the affected area
- Arm pain that is severe or increasing after an arm lift
- Swelling that is so severe, it limits your ability to move your arm
- Severe pain that doesn’t seem to improve with prescribed medication
- Numbness, tingling, weakness, or loss of sensation in the affected arm or hand
How is compartment syndrome diagnosed?

A medical provider will conduct a physical exam and ask about the symptoms you are experiencing. When compartment syndrome is suspected, the provider may place a needle into the affected area to measure the pressure inside the compartment. The needle attaches to a pressure meter, which shows whether the pressure is normal or high. If it’s too high, treatment may be needed to relieve the pressure.
How is acute compartment syndrome treated?
If an arm lift patient is diagnosed with acute compartment syndrome, emergency surgery is scheduled. The surgeon may perform a fasciotomy, which involves cutting the fascia open to relieve pressure. It’s important not to delay the surgery; Permanent nerve damage can happen within just 12 to 24 hours of onset. Muscular damage can occur even faster.
Is acute compartment syndrome curable?
The prognosis is generally excellent for most patients who seek treatment early. The nerves and muscles inside the compartment usually recover well after fasciotomy.
What is the prognosis for acute compartment syndrome?
Long-term outcomes are usually good if the patient receives immediate treatment. Factors such as what caused the injury and the severity of the injury can play into the patient’s prognosis.
Is acute compartment syndrome life-threatening?
Acute compartment syndrome is a major complication that can be fatal if not untreated. We spoke to Dr Bernard Beldholm, a specialist surgeon offering body contouring and arm lift surgery in Newcastle. Although he has never had a patient develop compartment syndrome during his more than 15 years as a surgeon, he emphasised the importance of getting treated immediately.
‘Acute compartment syndrome can be life-threatening if left untreated. If pressure within the muscle compartment gets too high, it can reduce blood flow in the area. Without fresh oxygen and nutrients supplied by the bloodstream, the muscles and nerves can become damaged **. Necrosis of the skin or tissues might result, which could cause a painful or life-threatening infection. Amputation could be needed in severe cases. The good news is arm lift patients that receive immediate medical attention usually recover well,‘ he says.
What happens if acute compartment syndrome is left untreated?
Acute compartment syndrome must be treated immediately. Delaying treatment even just 12 to 24 hours can cause permanent nerve or muscle injuries. Deformities might also occur. For example, if a patient has acute compartment syndrome in their forearm and doesn’t seek treatment, they may develop Volkmann ischemic contracture. Volkmann ischemic contracture is a disfigurement of the hand, fingers, and wrist caused by an injury to the forearm muscles.

Wrist fusion for Volkmann’s ischaemic contracture (Using Synthes fusion plate) Surgical Technique – OrthOracle
What should you do if you suspect you have acute compartment syndrome after an arm lift?
Acute compartment syndrome is a medical emergency. Call your surgeon and see a doctor right away if you have signs of compartment syndrome. Do not delay, or you could risk permanent limb damage or amputation. Raise the affected limb above heart level and loosen any bandages or compression garments if they are too tight in the meantime.
Case Report: 84-Year-Old Woman Develops Compartment Syndrome After an Injury
The Orthopaedic Surgery journal investigates a case report involving an 84-year-old woman with compartment syndrome. (Ref 2) The woman came to the emergency department complaining of severe pain in her right upper arm that had lasted 24 hours. Her hand hung limply, and she wasn’t able to flex her fingers like she normally could. A week earlier, she had suffered a minor hit to her upper arm, which caused a haematoma.
She initially had no pain, but six days after the incident, she noticed unusual swelling and severe pain on her anterior upper arm. Pain medication wasn’t helping. Doctors suspected she had compartment syndrome in her upper arm.
A surgeon performed a total fasciotomy with an antero‐lateral incision to relieve the pressure. They extracted a total of 200 ml of blood. Luckily, the surgeon was able to close the skin layer without requiring a skin graft.
One day after the fasciotomy operation, she regained normal sensation in her arm and hand. She was also able to flex her fingers. Within three months, her motor function was close to normal.
FAQs
What will happen if I don’t seek treatment for acute compartment syndrome?
Compartmental swelling causes pressure that can constrict blood flow to the limbs. Swelling that lasts a long time can eventually cause permanent injury to the nerves and muscles. Patients who don’t see a doctor right away may eventually lose mobility or require amputation of the affected limb.
What other complications are possible after arm lift procedures?
Major complications such as acute compartment syndrome, nerve injuries, severe wound dehiscence, infections, excessive bleeding, brachial muscle injury, and pulmonary embolism are rare.
Minor complications can include small wound separations (wound dehiscence), temporary sensory loss as the damaged nerves heal, pinpoint bleeding, brachioplasty scar contracture, hypertrophic scars, asymmetry, etc. Concomitant procedures (i.e. having multiple surgeries in one day) can increase the risk of complications. Minor complications are more likely to happen than major ones.
No surgeon can guarantee a surgeon free of complications. Still, it’s important to choose a highly experienced surgeon for your arm lift procedure. That way, if complications happen, they will be better equipped to treat them. Your surgeon should provide you with an informed consent listing the possible complications before you agree to have surgery.
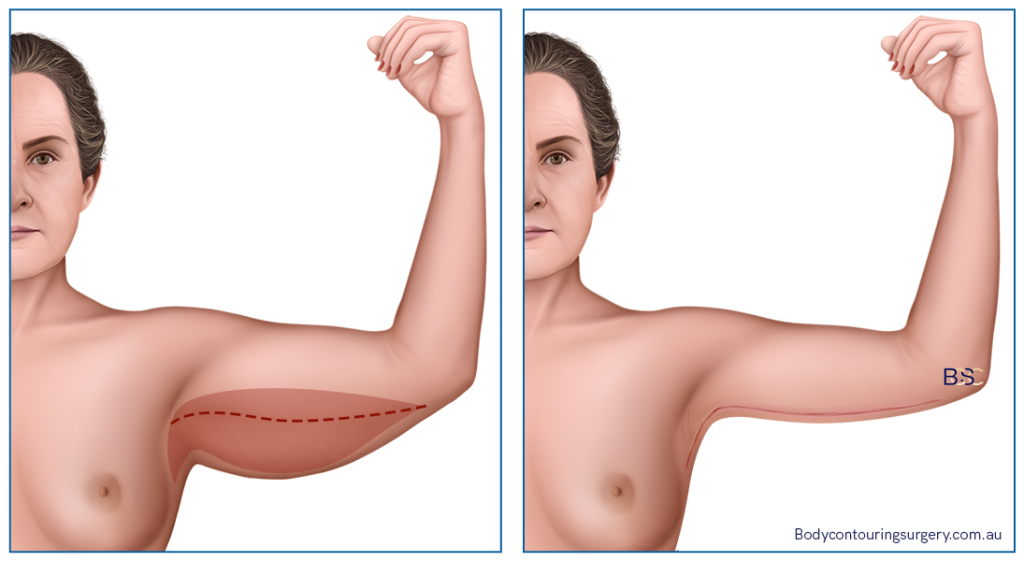
Who is the typical arm lift patient?
This surgical procedure is suitable for patients with excess skin on their upper arms. Typically, people have the surgery after massive weight loss. Massive weight loss is generally considered losing 45 kilos, or half of a person’s body weight. Anyone wishing to tighten ** arms after bariatric surgery or extreme dieting may be eligible so long as they do not smoke, are healthy, and are not nursing or pregnant.
I’m considering an arm lift. What’s my next step?
To learn if an arm lift is right for you, book a consultation with a surgeon that specialises in body contouring. They will conduct a physical examination and ask about your medical history and lifestyle to determine if arm contouring is appropriate. We spoke to Dr Bernard Beldholm, who has performed hundreds of arm lift surgeries over the years. He says patient selection is critical to a ** and successful surgery.
Why does bariatric surgery cause loose skin?
**, massive weight loss causes a person’s body size to shrink, but the skin doesn’t always shrink with it. The skin often appears ** and deflated once the excess weight is gone. Upper arm contouring and related operations like tummy tucks or thigh lift surgery are just a few of the body contouring procedures available to the massive weight loss patient.
References
- Compartment Syndrome. (2022). Pennmedicine.org. https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/compartment-syndrome
- Orthop Surg. 2013 Aug; 5(3): 229–232. Published online 2013 Aug 12. doi: 10.1111/os.12054
- Malik, A. A., Khan, W. S. A., Chaudhry, A., Ihsan, M., & Cullen, N. P. (2009). Acute Compartment Syndrome – a Life and Limb Threatening Surgical Emergency. Journal of Perioperative Practice, 19(5), 137–142.