Recovering From Belt Lipectomy (Lower Body Lift)
At Body Contouring Surgery Clinic (BCSC), our recovery programs for belt lipectomy (body lift) are structured, evidence-based, and designed to support patients after lower-body lift (Belt lipectomy) surgery. This surgical procedure removes excess skin and tissue from the lower abdomen, flanks, back, and buttocks, typically after significant or massive weight loss or bariatric surgery.
Patients often present with functional symptoms, hygiene concerns or difficulty with clothing. Circumferential removal of excess skin folds helps reshape the lower torso and targets functional issues. Research shows that body contouring after major weight reduction can treat physical functioning and quality of life (1).
Belt lipectomy
What Is a Belt Lipectomy (Body Lift)?
A belt lipectomy is a major body-contouring procedure involving circumferential excision of tissue around the lower trunk. Excess skin and fat are removed from the abdomen, flanks, lower back and buttocks. This body lift surgery is ideal for patients with loose skin after massive weight reduction. In appropriate cases, it may be performed alone or in combination with:
- Tummy tuck (Abdominoplasty)
- Breast lift (Mastopexy) or breast reduction (Reduction mammoplasty)
- Thigh lift (Thighplasty)
- Liposuction (suction lipectomy)
Achieving a stable weight before belt lipectomy surgery is critical. Evidence shows better wound healing and fewer complications when weight is stable for at least six months (1).
Indications for Belt Lipectomy

Most belt lipectomy patients have undergone:
- Substantial weight loss
- Major weight loss from lifestyle changes
- Bariatric surgery
- Skin redundancy that cannot contract naturally
Studies show that substantial weight loss can result in redundant folds that affect hygiene, physical activity, and comfort (2). Belt lipectomy specifically targets the circumferential lower trunk, providing a more complete solution than abdominoplasty alone.
Preparing Your Home and Support System
What to Do 1 Month Before Surgery
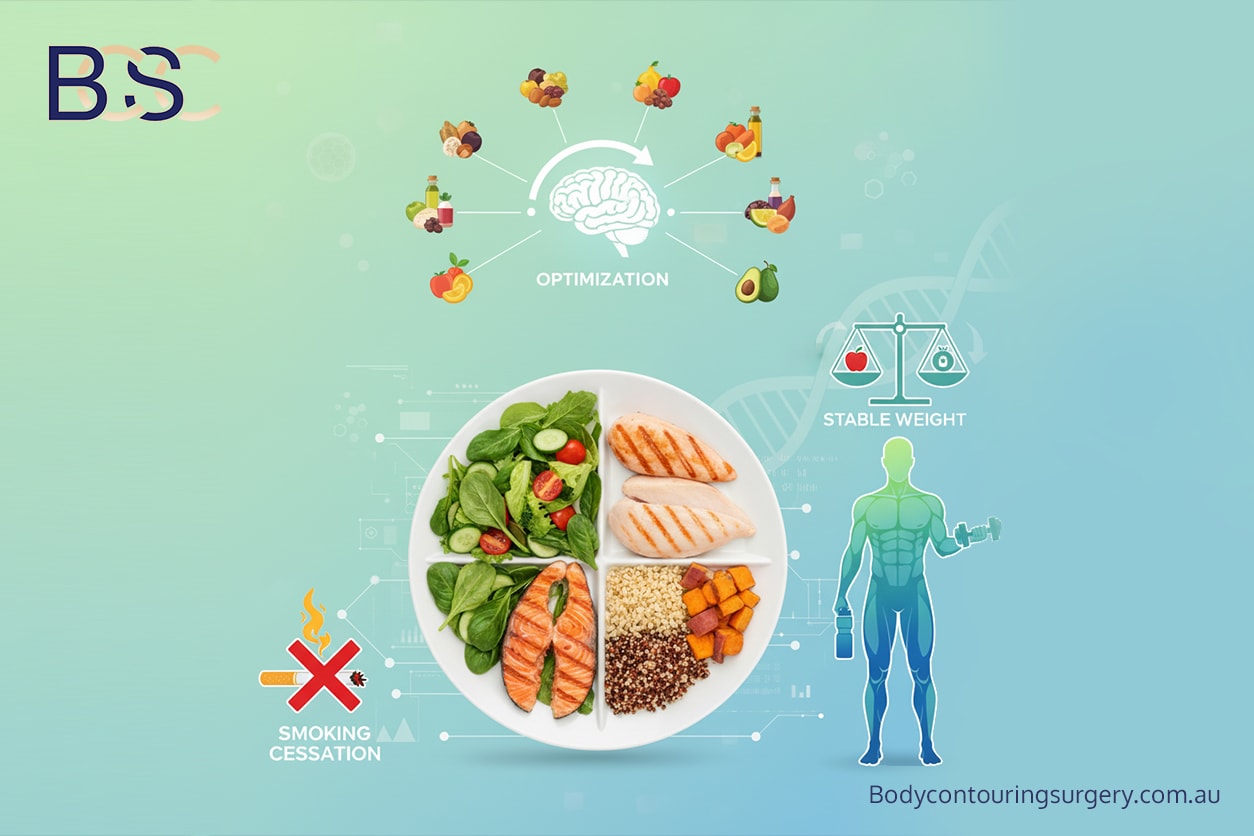
At one month out, preparation focuses on optimising your health and home environment:
- Ensure your weight remains stable, as weight fluctuations can impair healing.
- Continue a balanced diet rich in protein, iron, zinc and vitamins.
- Discuss all medications and supplements with your healthcare provider.
- Stop smoking and avoid nicotine products, as these increase wound‑healing risks.
- Arrange time off work and confirm your support person for the first 1–2 weeks.
- Organise childcare, pet care, and household support.
- Begin gentle walking if tolerated to build baseline fitness.
What to Do 2 Weeks Before Surgery
At this stage, final planning and safety checks occur:
- Finalise postoperative support, including help with meals and transport.
- Prepare your home recovery space (pillows, recliner, bedside supplies).
- Avoid anti‑inflammatory medications unless approved.
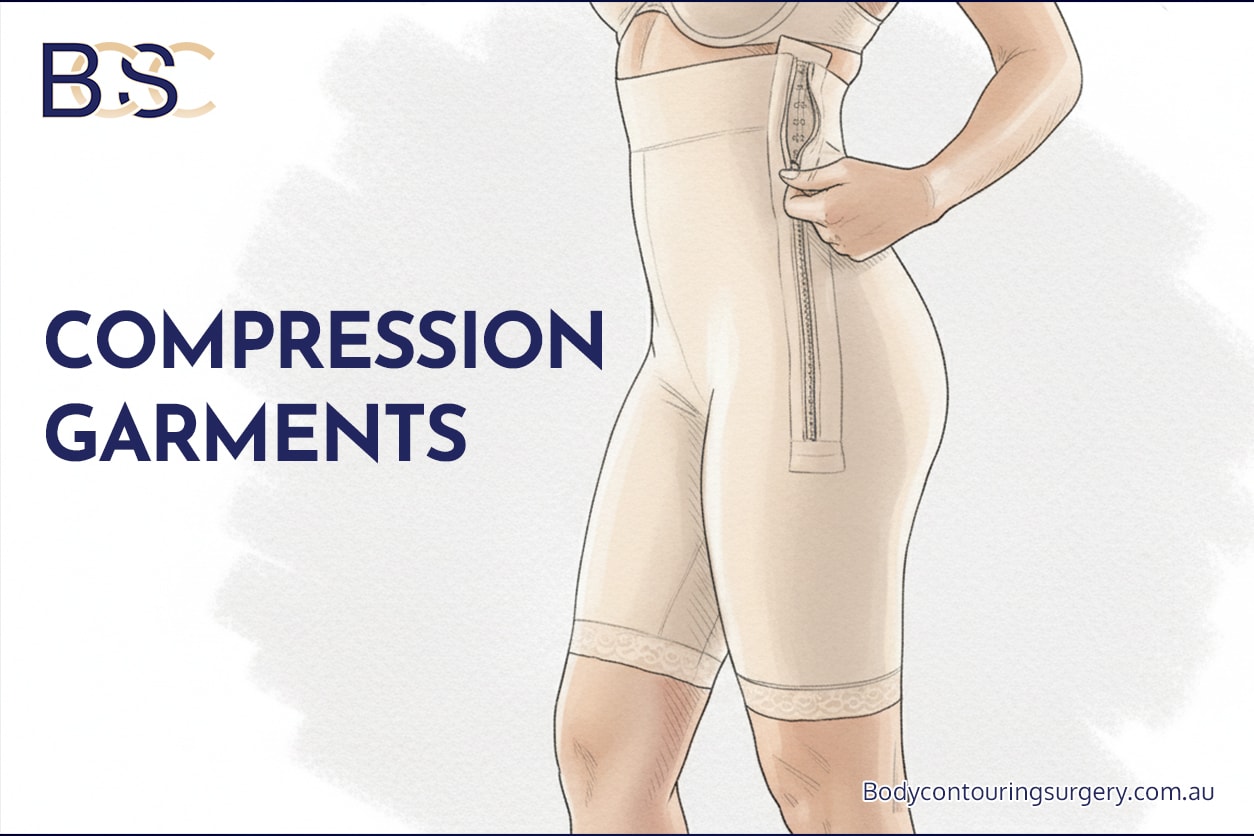
- Ensure compression garments have been ordered or are ready for use.
- Reduce heavy physical activity to avoid pre‑surgery fatigue or strain.
- Review hospital instructions, fasting guidelines, and arrival times.
What to Do 1 Week Before Surgery
This week centres on smoothing the transition into hospital care:
- Confirm hospital booking and bring the required documents.
- Prepare easy‑to‑reach clothing and toiletries for your hospital bag.
- Cook and freeze several meals for the first two postoperative weeks.
- Ensure your home is free of tripping hazards and that pathways are clear.
- Set up a shower chair and non‑slip mats if needed.
- Continue gentle walking to support circulation.
What to Do the Day Before Surgery

- Follow the hospital’s fasting instructions closely.
- Move to a clear‑fluid diet if instructed (especially for patients on GLP‑1 medications).
- Shower with antibacterial wash if recommended.
- Remove all jewellery and nail polish.
- Pack your compression garments for use immediately after surgery.
- Go to bed early and rest.
Support during the first few weeks is essential, and thoughtful preparation can facilitate early recovery. Preparing your home in advance helps reduce physical strain, promotes rest, and supports wound healing. Consider the following steps:
- Arrange assistance with meals, household tasks, and childcare. Most patients find bending, lifting, and prolonged standing difficult in the early period.
- Plan a quiet, comfortable recovery space with easy access to the bathroom, supportive pillows, and, if possible, a recliner or adjustable bed.
- Pre-prepare nutritious meals that support a balanced diet and adequate protein intake, which is important for wound healing.
- Set up essential items within easy reach, such as water, medications, dressings, phone chargers, and compression garments.
- Avoid heavy lifting or demanding activities for several weeks to avoid placing tension on the surgical site.
- Ensure early mobilisation, as walking short distances while supported is important to reduce the risk of blood clots.
- Organise transport for follow-up appointments, particularly during the first two weeks, when driving is not recommended.
- Prepare the bathroom by adding nonslip mats, grab rails, or a shower chair as needed.
- Arrange care for pets in advance, including assistance with walking, feeding, or lifting animals.
- Follow all the surgeon’s instructions to reduce risk, including fasting guidelines, medication adjustments, and preparing your compression garments for use immediately after surgery.
GLP‑1 Medications and Surgery
For patients using GLP‑1 medications (such as semaglutide, liraglutide, tirzepatide, and dulaglutide), additional preparation helps reduce the risk of delayed gastric emptying during general anaesthesia. These medications can slow digestion, which may increase the risk of aspiration if the stomach is not adequately emptied before surgery.
Key Instructions
- Continue GLP‑1 therapy unless your anaesthetist advises otherwise. Current guidance recommends continuing these medications for most patients.
- Follow a strict 24‑hour clear‑fluid diet before surgery. This helps ensure your stomach empties properly.
- Fast for at least 6 hours before arriving at the hospital.
- Attend your pre‑operative anaesthetic assessment, where the care team will confirm your medication schedule and assess for symptoms of slowed gastric emptying (such as nausea, vomiting, or persistent fullness).
What You Can Consume on a 24‑Hour Clear‑Fluid Diet
A clear‑fluid diet includes liquids you can see through. These pass through the stomach more quickly.
Allowed clear fluids:
- Water (still or sparkling)
- Clear broth or consommé (no solids)
- Apple juice or white grape juice
- Electrolyte drinks (avoid red or purple colours if possible)
- Weak black tea or black coffee (no milk)
- Clear jelly (yellow or green varieties)
- Ice blocks made from allowed fluids
Avoid:
- Dairy products (milk, yoghurt, smoothies)
- Protein shakes
- Soups with solids or cream
- Purees or blended foods
- Soft drinks with pulp or cloudy appearance
- Any solid food
Why This Matters
Following these instructions helps reduce the risk of aspiration under general anaesthesia.
If you experience nausea, vomiting, sudden abdominal pain, or severe bloating during the 24‑hour period, contact the hospital or surgical team for advice.
These steps reduce aspiration risk during general anaesthesia.
The Day Before Surgery
The hospital will usually contact you the afternoon before surgery to confirm your admission details. Depending on your position on the operating list, you will be given a specific arrival time. In most cases, patients are asked to arrive 1–2 hours before their scheduled surgery time. This allows staff to complete hospital check‑in, confirm paperwork, perform the anaesthetic assessment, and give your surgeon time to complete pre‑operative markings and final preparations.
The Day of Surgery
Admission
On arrival, staff complete identity checks, medical history review, consent confirmation, and baseline observations.
Anaesthetic Preparation
- Anaesthetist review
- IV cannulae insertion
- Surgical markings by Dr Beldholm
- Warming blanket for comfort
- TIVA general anaesthesia
- Urinary catheter placed once asleep
The Operation
A belt lipectomy generally takes 6–8 hours, depending on:
- Extent of excess skin
- Need for muscle repair
- Combined procedures
- Tissue characteristics
Drains are placed to remove excess fluid and protect the surgical site.
Hospital Stay & Early Recovery
Day 1 – The Most Challenging Day
Day 1 is often the most intensive part of your hospital stay. You will be recovering from general anaesthesia, closely monitored by nursing staff, and gradually introduced to early movement. This is also the day you will see your surgeon for a postoperative review.
What to Expect When You Wake Up
After surgery, you will wake in the recovery unit before being transferred to your hospital room. It is normal to experience drowsiness, disorientation, or cold. You may have the following in place:
- Drains to collect excess fluid from the surgical area
- PICO dressings to support the incision and reduce tension
- IV fluids to maintain hydration
- PCA (Patient‑Controlled Analgesia) for pain relief
- Calf compressors to reduce the risk of blood clots
- IDC catheter to drain the bladder without needing to stand early
- Incentive spirometer to support lung health after anaesthesia
Nursing staff will monitor your blood pressure, pulse, oxygen levels, temperature and overall comfort.
Surgeon Review

Your surgeon will see you in the morning to:
- Check your vital signs and overall well-being
- Assess the surgical site and dressings
- Review the drain function and output
- Review your pain levels
- Answer any early questions about your recovery
This assessment helps guide the next steps in your care.
Mobilisation and Early Movement
Low blood pressure, dizziness and nausea are common due to long anaesthesia and fluid shifts. Once you are stable:
- The IDC catheter may be removed when you are able to safely stand and walk with assistance.
- PCA may be discontinued once your pain is controlled and you transition to oral medication.
- IV cannulae may be capped, allowing you to move more freely.
You will be encouraged to sit up, stand, and take short assisted steps. This is important to reduce the risk of blood clots and support healthy lung expansion.
Eating and Drinking
Most patients begin with small sips of water, then light meals as tolerated. Nausea medication is available if needed.
Pain and Comfort Management
Pain will be present but manageable with:
- PCA or oral medication
- Gentle positioning and support pillows
- Minimal twisting or bending
Nursing staff will assist you with safe movement to avoid strain on the abdomen and lower body.
Day 1 is focused on stability, monitoring, and gentle mobilisation — setting the foundation for the days ahead.
Days 2–5
Most patients remain in the hospital for 3–5 days:
- Nurses review wounds and drains
- Mobility increases to prevent blood clots
- Compression garments fitted
- Pain managed with prescribed medications
Discharge occurs once mobilising, eating, and comfortable.
The First Few Weeks at Home

The first few weeks after a belt lipectomy are focused on wound healing, swelling control, infection prevention, and mobility. This period includes regular clinic visits, dressing changes, and close monitoring of your progress.
What to Expect in the First 1–2 Weeks
During this stage, your body is actively healing. You will likely experience swelling, tightness and fatigue. Support from the clinical team is essential.
You will need to:
- Wear compression garments 24/7 to reduce swelling and support the surgical site.
- Take prescribed medications as directed.
- Walk short distances regularly, ideally 4–6 times per day, to support circulation.
- Avoid strenuous activities, bending, twisting or lifting.
- Attend 2–3 clinic visits per week for wound checks and dressing care.
Dressing Care: PICO and Comfeel
Your dressings play a major role in wound protection and hydration during the early recovery phase.
- PICO dressings typically remain in place for the first week. At Day 7, you will attend the clinic for PICO removal and replacement with Hypafix or Comfeel dressings.
- Comfeel dressings (or similar hydrocolloid dressings) support moisture balance and protect fragile early wounds. These may need changing several times per week, depending on drainage, skin sensitivity and your surgeon’s instructions.
- Our nursing team monitors for skin irritation, signs of infection, or early wound separation.
Clinic Visits
You will be reviewed by the nursing team frequently, especially in the first two weeks. During these visits, the team will:
- Inspect the surgical site and monitor healing progress
- Change dressings (including PICO removal and Comfeel/Hypafix application)
- Provide LED light therapy to support healing
- Assess swelling and garment fit
- Check for early signs of wound separation or fluid collection
- Answer any concerns and adjust care instructions
Activity and Mobility
Continue gentle movement while avoiding strain:
- Short, frequent walks
- No heavy lifting or stretching
- Rest in a semi‑flexed position when lying down to protect the incision line
- Use pillows for support as needed
Nutrition for Optimal Healing

Eating well is essential during the early healing phase. Choose foods that support tissue repair and hydration:
Recommended foods:
- Lean proteins (chicken, fish, eggs, tofu)
- Protein smoothies (if tolerated)
- Iron‑rich foods (spinach, legumes, lean red meat)
- Fresh fruit and vegetables
- Whole grains
- Hydration: water, herbal tea, electrolyte drinks
Avoid:
- Highly processed foods
- Excess sugar or salt
- Alcohol (may interfere with healing and medications)
- Smoking or nicotine products
This early phase lays the foundation for subsequent stages of recovery. Close follow‑up and proper care during the first few weeks can help reduce complications and support a smoother healing process.
This stage focuses on wound healing, control of swelling, prevention of infection, and garment support.
Expect to:
- Wear compression garments 24/7
- Take prescribed medications
- Walk short distances regularly
- Avoid strenuous activities
- Attend 2–3 nurse visits per week
Wound separation is common. Published reports show dehiscence rates of 13–17%.
Weeks 4–8: Transition Phase
During this period:
- Swelling gradually resolves
- Light activity resumes
- Vigorous exercise avoided
- Silicone scar therapy begins
- Surgeon follow-up at one month
Nutrition and hydration remain important.
Long-Term Recovery

Most patients resume normal activities within 8–12 weeks. Final healing, including scar maturation, can take 12–18 months.
Key factors:
- Maintaining a stable weight
- Avoiding weight fluctuations
- Hydration and a balanced diet
- Protecting scars from the sun
- Gradual return to physical activity
Studies consistently report high patient satisfaction after circumferential body contouring (1).
Risks & Complications
Common risks include:
- Wound dehiscence (13–17%)
- Seroma (up to 13%)
- Hematoma (2–4%)
- Skin necrosis (3–5%)
- Infection (3–9%)
- Rare pulmonary complications
Overall complication rates for circumferential procedures range from 30–44%, with most being minor.
Recovery Timeline Summary
_-_Infographic.jpg)
Belt lipectomy recovery timeline infographic
Follow-Up Care

Regular follow-ups allow monitoring of:
- Wound healing
- Drain removal
- Garment fit
- Scar progress
- Swelling
- Activity progression
Report any concerning symptoms immediately.
Healthy Lifestyle After Surgery
Maintaining results requires:
- Balanced nutrition
- Avoiding major weight changes
- Safe exercise routines
- Hydration
Frequently Asked Questions
How long does it take to recover from a belt lipectomy?
Most patients return to light activities within 4–6 weeks, with full recovery typically occurring around 3 months.
How long to wear compression garments?
Generally, 6–8 weeks.
How long does swelling last after a lower body lift (belt lipectomy)?
Early swelling typically resolves within 4–6 weeks; residual swelling may persist for 3–6 months.
- El-Gharbawi AH, El-Sabbagh AH, Shouman OO, et al. Postbariatric Abdominal Contouring: Technical Approach and Quality of Life. Plast Reconstr Surg. 2022;150(4):796–803.
- Van Huizum MA, Roche NA, Hofer SOP. Circular Belt Lipectomy: A Retrospective Follow-up Study on Perioperative Complications and Cosmetic Outcome. Ann Plast Surg. 2005;54:459–464.
- Carloni R, De Runz A, Chap