Umbilical Hernia Repair during Fleur-de-Lis Abdominoplasty Surgery
Though umbilical hernias, which are highly prevalent in babies, are painless and commonly go away on their own, sometimes, when adults experience them, they may be tender to the touch, cause discomfort, and can be aesthetically unappealing.
A common indication of an umbilical hernia is a bulge around the navel. Most patients report seeing a protrusion when they sneeze or lift something heavy. Fleur-de-Lis Abdominoplasty offers adults with an umbilical hernia more than just aesthetic benefits, it presents a unique opportunity for simultaneous umbilical hernia repair and removal of fatty tissue and skin excess on the upper and lower abdomen resulting from extensive weight loss.
Many massive weight loss patients, particularly postpartum women, may also suffer from weakened abdominal muscles. FDL surgery offers combined benefits: creates abdominal contour, repairs separated abdominal muscles, targets significant excess skin on the lower and upper abdomen after a C-section, and repairs umbilical hernias.
What is an Umbilical Hernia?
What is an Umbilical Hernia?
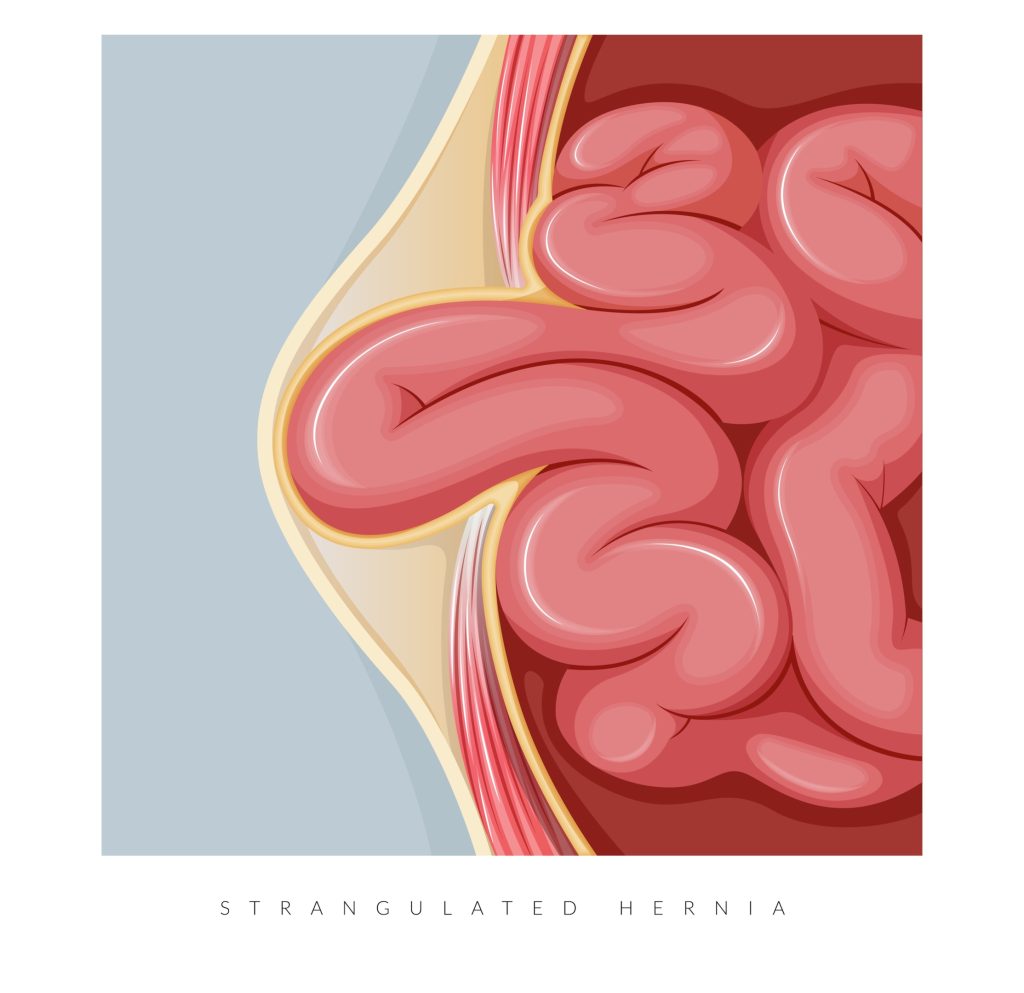
The type of hernia depends on its location within the abdomen. An umbilical hernia, which is located near the umbilicus or belly button, is caused by abdominal fluid collection, multiple pregnancies, or obesity. Weakness in the abdominal wall can cause internal organs, such as intestines to push against the skin, resulting in a noticeable bulge, especially when coughing or straining. The protruding organs push against the skin, creating a noticeable swelling around the navel.
According to a study by NCBI, “[u]mbilical hernias are three times more common in women due to the effects of pregnancy and childbirth, as well as the increased incidence of obesity.”

Asymptomatic vs Symptomatic Hernia
Asymptomatic vs Symptomatic Hernia
An asymptomatic hernia has no symptoms other than the bulging. They can be large or small. This type of hernia is normally diagnosed during a general check-up. It is usually easily reducible, meaning it can be easily pushed back in. It will usually come out when the patient is straining.
Symptomatic Hernia
A symptomatic hernia is indicated by discoloration of the bulging area, sharp pain in the abdomen, or nausea. Surgical repair is recommended for such hernias, especially when they increase in size, to prevent bowel obstruction or hernia strangulation, which can lead to sepsis.
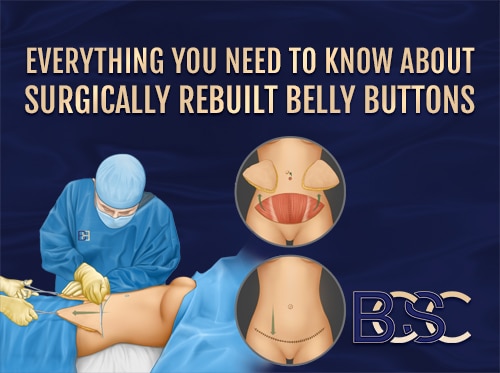
Umbilicoplasty
Often performed to repair an umbilical hernia, umbilicoplasty is a procedure performed by FRACS surgeons to repair the appearance of the belly button. Commonly performed out of medical necessity, especially if there is hernia strangulation, the procedure is generally classified as a medical, rather than a cosmetic, surgery.
Many postpartum patients who experience a protrusion in their navel area, experience discomfort and pain. In rare instances when the belly button is missing due to agenesis or damage during pregnancy, specialist surgeons reconstruct the navel using neo-umbilicoplasty.
Neo-umbilicoplasty, also known as belly button reconstruction, is a cosmetic procedure aimed to reconstruct or reshape the navel. It is commonly performed during a traditional abdominoplasty (tummy tuck procedure) to change the appearance of the belly button. Most experienced surgeons use the four-flaps technique to reconstruct a new umbilicus. According to a study published by NCBI notes, “[t]his method uses the neighbouring tissue by simply elevating four-flaps and can yield sufficient depth and an aesthetically pleasing shape with appropriate superior hooding.”
Ideal neo-umbilicoplasty candidates are patients with a stable weight and are non-smokers. Most surgeons advise against those who do use tobacco products (vapes, cigarettes, chewing tobacco) to refrain from smoking for six weeks before and after surgery to ensure optimal recovery. Before you undergo fleur de lis surgery combined with neo-umbilicoplasty, consult a specialist surgeon like Dr. Bernard Beldholm for a tailored surgical plan.
Benefits Of Umbilicoplasty
Most patients seek umbilicoplasty for the following reasons:
Minimal Invasiveness
Umbilicoplasty is usually a day procedure and has low complication rates.
Eliminates Multiple Anaesthesia Events
Due to low complication risk, umbilicoplasty can be performed with other procedures, like abdominoplasty surgery, significantly reducing the recovery time and eliminating the need for multiple anaesthesia events.
Relieves Pain and Discomfort
The surgery alleviates symptoms of umbilical hernia, such as pain and discomfort.
Minimal Scarring
Umbilicoplasty requires small incisions, which results in scarring.

What is Fleur-de-Lis Abdominoplasty?
What is Fleur-de-Lis Abdominoplasty?
Fleur-de-Lis Abdominoplasty is a specialised variation of traditional tummy tuck (Abdominoplasty) surgery that results in tighter skin, a more contoured shape, and the elimination of skin laxity. It is performed on postpartum patients or those who have experienced significant weight loss due to diet, exercise, or gastric bypass surgery. The surgery treats loose skin around the abdomen to achieve a contoured midsection. During FDL surgery (tummy tuck) (Abdominoplasty), the surgeon removes loose skin by making both horizontal and vertical incisions to tighten as much skin as possible.
Post-pregnancy Fleur-de-Lis surgery requires excess abdominal skin tightening, which could lead to displacement of the belly button. To ensure optimal results, most surgeons perform Fleur-de-Lis abdominoplasty in conjunction with umbilicoplasty.
Benefits of Combined Surgery

Umbilicoplasty and fleur de lis abdominoplasty
Apart from the aesthetic results obtained from the procedure, there are a few other benefits of combining Fleur-de-Lis abdominoplasty surgery with umbilicoplasty, such as:
- Single Anaesthesia Event: Like other type of invasive surgery, including extended abdominoplasty and traditional abdominoplasty, a fleur de lis tummy tuck (Abdominoplasty) involves the use of general anaesthesia, which has side effects like drowsiness, sore throat, and confusion. Combining FDL and umbilicoplasty reduces the number of times a patient has to experience these effects. The costs associated with anaesthesia will be lessened as patients will only pay for it once when they would otherwise have to pay twice for two separate procedures.
- Reduced Risks: It is common for surgical patients to develop complications like infection, blood loss, or hematoma. However, combining the procedures reduces risk potential.
- Less Downtime: Every patient is eager to get back to their daily activities after surgery. If a patient decides to have umbilicoplasty and FDL (Abdominoplasty) separately, more downtime will obviously be involved. A combined surgery allows for less lost time from work and reduces time spent away from caring for children, pets, and everyday responsibilities.
- Comprehensive Results: When Fleur-de-Lis is Abdominoplasty combined with umbilicoplasty, the results are more aesthetically pleasing since the surgeon can address multiple issues simultaneously. The surgical site will likely heal faster, there will likely be less scarring, and the umbilicus will likely **.
- Optimised Recovery: A combined procedure means there will be a single recovery period. Most patients find extended recovery time to be difficult due to the physical restrictions that come after a surgical procedure.
- Lower Cost: With a combined surgery, patients only need to pay for one surgical procedure, a single hospital fee, and one anaesthetist fee, which can drastically reduce overall costs. Costs related to travelling back and forth for follow-up and aftercare visits are also minimised. From a financial standpoint, undergoing a combined procedure is more economically sound than having two separate surgeries.
Surgical Procedure
Surgeons make a plan that they follow during the combined procedure to ensure a successful outcome. Below are some of the steps involved.
Anaesthesia

During the surgery, an anaesthetist administers general anaesthesia. The amount of medicine administered depends on the duration of the surgery, the paients’ tolerance to medication, and the client’s medical history. It is vital to inform the surgeon of any anaesthesia allergies to prevent complications during the procedure. The administered anaesthesia will keep the patient unconscious through the procedure to avoid pain and trauma.
A tube is placed in the airway to help the patient breathe while under anaesthesia.
Incision
After anaesthesia, the general surgeon makes horizontal and vertical incisions for a combined FDL, umbilicoplasty, and hernia repair. The horizontal incision is made on the lower abdomen below the pubic line, while the vertical incision runs up to the sternum.
Umbilicoplasty
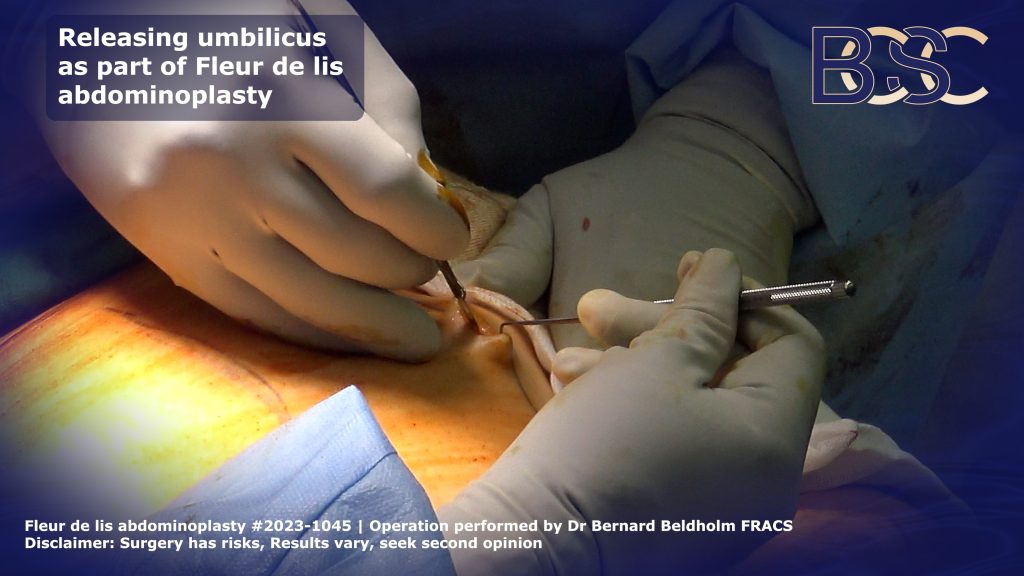
Releasing the umbilicus as part of a Fleur de lis abdominoplasty | BCSC
After the incisions, the surgeon reshapes the umbilicus. This is achieved by removing any excess skin and fat around the navel to create a more desirable shape. Most patients prefer an innie to an outie. This helps to accommodate most of their clothes and allows patients to stay on-trend. The position and shape of the umbilicus are essential since it is the central part of the abdomen.
Hernia Repair
After the umbilicoplasty, the surgeon identifies the hernia sac and gently pushes it back to its original place. The gap where the hernia appeared is reinforced with a mesh supported by the neighbouring healthy tissues to ensure no hernia recurrence.
FDL Abdominoplasty
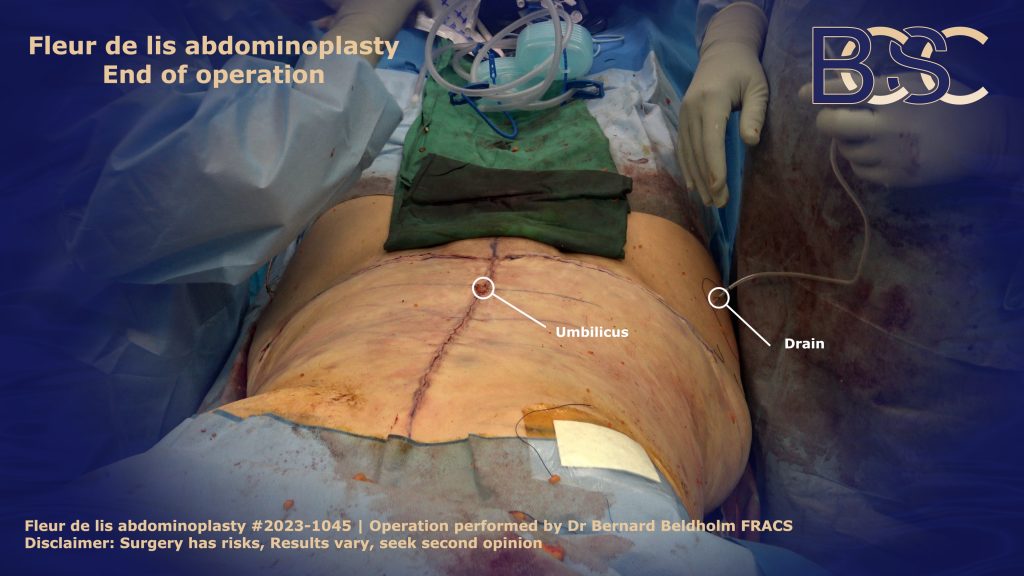
Fleur de lis abdominoplasty end of operation showing incisions | BCSC
During this step, the surgeon removes excess skin and fat by dissecting the lower and upper abdomen. If the weakened abdominal muscles have separated from the Linea alba (diastasis recti), the surgeon repairs them using strong sutures. The amount of loose abdominal skin removed depends on the patient’s skin laxity and their personal goals.
Closure
The surgeon then closes the incisions, starting with the deepest tissues. Most surgeons use strong, absorbable sutures that eventually dissolve in the body without causing any harm. When necessary, the surgeon places surgical drains to reduce fluid accumulation. The surgeon then closes the outer skin with the new umbilicus, ensuring it is centrally positioned for optimal results.
Drains
Surgical drains are plastic tubes inserted into the body after surgery. They are placed near the incision site to remove excess fluids that collect under the skin. Drains are used to prevent the formation of seromas or haematomas which could delay healing and reduce the risk of infection. Though they are required for some surgeries, drains are limiting for patients.
Umbilical Hernia Repair/Fleur-de-Lis Abdominoplasty Recovery
For a smooth recovery, surgeons provide patients with guidelines after surgery to aid in a recovery. Below is what to expect.
- Hospital Stay: It is risky to drive home after invasive surgery like Fleur-de-Lis abdominoplasty because sudden movements can cause trauma to the fresh incision site. General surgeons advise a hospital stay of at least 1 to 2 days for regular monitoring and professional care. During this time, the medical team observes the healing of the patient’s wound and adjusts the post-operative instructions.
- Pain Management: After the surgery, when the effects of the anaesthesia wear off, the patient experiences moderate pain. The surgeon will prescribe pain medication to ease the transition back to daily routines. Pain medication also helps patients recover faster by mitigating discomfort and giving them enough relief to be able to take short walks.
- Activity Restrictions: A patient should not engage in certain activities while recovering from the surgery. In the first few days after the combined procedure, they are expected to take light walks to avoid the formation of deep-vein thrombosis. The surgeons also advise against taking a full shower after the surgery until the removal of the wound dressings to prevent infection. Dr. Beldholm, a FRACS surgeon with over 15 years of experience, instructs patients on how to set up their beds to ensure they don’t put too much pressure on the wounds, causing them to reopen.
- Follow-Up: For a smooth recovery, patients adhere to all postoperative instructions including attending regularly scheduled check-ups and wearing a compression garment to ensure the wound is healing nicely. During the check-ups, the surgeon will check drain levels and colour and remove the wound dressing when the time is right. Many patients don’t go for their check-up appointments because they feel fine. However, underlying issues that could cause poor wound healing can surface, and go unnoticed, resulting in complications such as infection, excessive fluid retention, and visible, unappealing scarring.
- Scar Care: Experienced specialist general surgeons use surgical techniques that are likely to reduce scarring during the procedure, such as absorbable sutures and PICO negative pressure dressings. However, scar care is essential for aesthetic results. Dr. Beldholm advises keeping your wound clean and avoiding direct sun to prevent your scar from becoming hyperpigmented.

Risks and Potential Complications of FDL and umbilicoplasty combined surgery
Risks and Potential Complications
Risks and potential complications are part of every surgical recovery journey. To ensure that you experience fewer post-op complications, it’s important to take proper care of the incision site and avoid heavy lifting.
Infection
Infection is a common occurrence post-surgery. Patients are advised to handle the wound dressing with clean hands and empty the drains as advised by their surgeons. Infection can delay the healing process and result in a raised scar, leading to unsatisfactory results.
Seroma
After an intrusive major surgery like FDL, tissues surrounding the incision site may get damaged, disrupting the drainage system. Excess fluid may build up under the skin, causing discomfort and infection if not drained.
Recurrence of Hernia
There are various causes of recurrent hernia, such as persistent cough, infections, and a larger-sized hernia. Strenuous activities before the patient fully recovers could also weaken the abdominal walls and lead to a recurrence.
Scarring
After a surgical procedure, scars are expected and normal. Specialist surgeons make horizontal incision cuts on the bikini line, where they are not easily visible. Though the vertical scar is more difficult to disguise, scarring often fades over time as long as the patient follows post-surgery wound care and adheres to instructions.
Long-Term Results
The long-term results of the combined surgery depend on how well the patients follow post-op directions and maintain a healthy lifestyle after the procedure. Patients who stick to a balanced diet, exercise regularly, and refrain from smoking are more likely to enjoy their results for years. Besides the aesthetic appearance, a repaired hernia allows patients to return to their normal routines more comfortably.
What if I Get Pregnant Again?
Getting pregnant after a combined fleur-de-lis and umbilicoplasty surgery is not dangerous for you or your baby. However, surgeons generally recommend a waiting period of 12 months to give the body enough time to heal and avoid muscle separation. The only downside to subsequent pregnancies after this procedure is that results could be compromised. Patients are advised to inform their surgeons about any plans to get pregnant in the future before their surgery. To learn more about pregnancy post-Fleur-de-lis procedure, check Dr. Beldholm’s article: 8 Concerns About Pregnancy After Fleur-De-Lis Abdominoplasty (Tummy Tuck) Surgery.

Dr. Bernard Beldholm, Top FRACS Surgeon in Australia, specialising in post-pregnancy and post-gastric bypass surgery body contouring surgery
Dr. Beldholm’s Bottom Line
It is common to develop umbilical hernias post-pregnancy or after significant weight loss. The size of the hernia determines the kind of procedure each patient undergoes. A combined FDL and umbilicoplasty procedure has many benefits, including long-lasting results, reduced downtime and risk potential, lower overall costs, and optimal results.
Therefore, it is important to book a consultation with an experienced FRACS surgeon who provides their patients with a tailored plan that accommodates their surgical goals, medical needs, and lifestyle factors.
References
- Coste, A. H., Jaafar, S., & Parmely, J. D. (2020). Umbilical Hernia. PubMed; StatPearls Publishing.
- Lee, Y. T., Kwon, C., Rhee, S. C., Cho, S. H., & Eo, S. R. (2015). Four Flaps Technique for Neo Umbilicoplasty. Archives of Plastic Surgery, 42(03), 351–355.
- Christopher, A. N., Morris, M. P., Patel, V., Davis, H., Broach, R. B., & Fischer, J. P. (2021). A Comparative Analysis of Fleur-de-Lis and Traditional Panniculectomy after Bariatric Surgery. Aesthetic plastic surgery, 45(5), 2208–2219.
- Gardani, M., Palli, D., Simonacci, F., Grieco, M. P., Bertozzi, N., & Raposio, E. (2019). Umbilical reconstruction: different techniques, a single aim. Acta Bio Medica: Atenei Parmensis, 90(4), 504.
- Geoffrey E Hespe, David M Stepien, Rami D Sherif, Robert H Gilman, Umbilicoplasty in Abdominoplasty surgery: Modifications for Improved Aesthetic Results, Aesthetic Surgery Journal Open Forum, Volume 3, Issue 3, September 2021, ojab025,
- Mendes, F. H., Donnabella, A., & Fagotti Moreira, A. R. (2019). Fleur-de-lis Abdominoplasty and Neo-umbilicus. Clinics in plastic surgery, 46(1), 49–60.
- Hesselink, V. J., Luijendijk, R. W., de Wilt, J. H., Heide, R., & Jeekel, J. (1993). An evaluation of risk factors in incisional hernia recurrence. Surgery, gynaecology & obstetrics, 176(3), 228–234.
- Zhitny, V. P., Young, J. P., & Stile, F. (2022). Recognition and repair of an incidental umbilical hernia repair during abdominoplasty. Annals of Medicine & Surgery, 82.
- Mitchell, R. T., & Rubin, J. P. (2014). The Fleur-De-Lis abdominoplasty. Clinics in plastic surgery, 41(4), 673–680.
- Mendes, F. H., Viterbo, F., & Moragas, W. R. (2024). Finesse in Fleur-de-lis Abdominoplasty. Clinics in plastic surgery, 51(1), 81–93.
- Ciudad, P., Manrique, O. J., Bustos, S. S., Pafitanis, G., Forte, A. J., Huayllani, M. T., Boczar, D., Vargas, M., Escalante, S., Parra Pont, L., Bustamante, A., & Chen, H. C. (2020). The Modified Extended Fleur-De-Lis Latissimus Dorsi Flap for Various Complex Multi-directional Large Soft and Bone Tissue Reconstruction. Cureus, 12(2), e6974.
- Kulaçoğlu H. (2015). Current options in umbilical hernia repair in adult patients. Ulusal cerrahi dergisi, 31(3), 157–161.