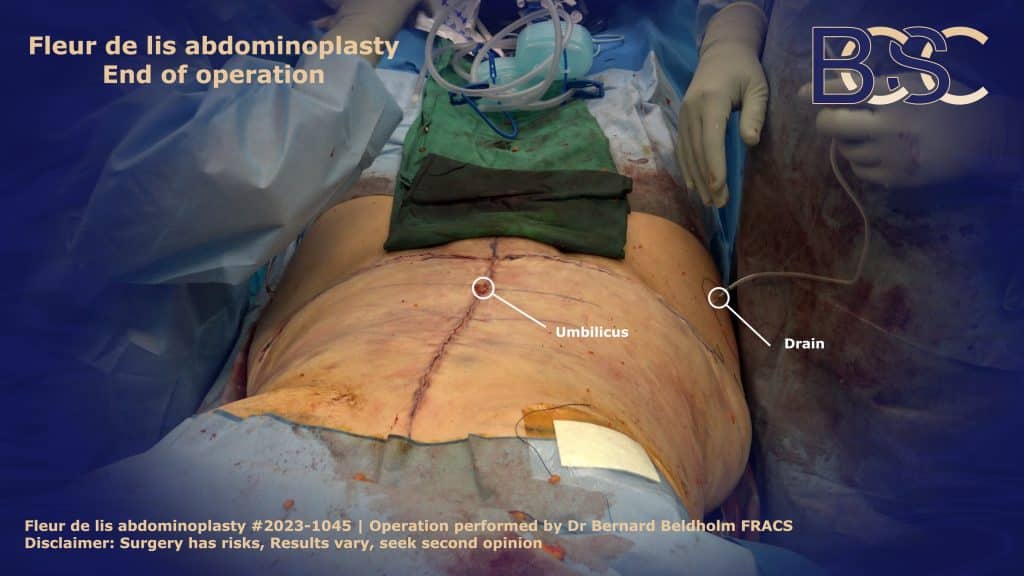
Risk of Outer Scar Following Fleur-de-Lis Surgery Abdominoplasty
Most individuals undergo Fleur-de-Lis abdominoplasty to target their abdominal contour. However, one should not overlook the risks associated with the procedure and all other surgical procedures. One such risk is scarring after Fleur-de-Lis abdominoplasty. It’s important to note that you cannot avoid scars in totality after a surgical procedure. There are ways, however, to make them less conspicuous and reduce the risk of abnormal scarring.
The patient also has a role to play. Therefore, learning about scarring following Fleur-de-Lis Abdominoplasty, how to reduce the risk, and what treatment options are available are crucial. If this seems too complicated and challenging, don’t worry. This guide covers everything you need to know regarding the risk of outer scar following fleur-de-lis abdominoplasty surgery.
Fleur-de-Lis Procedure After Massive Weight Loss
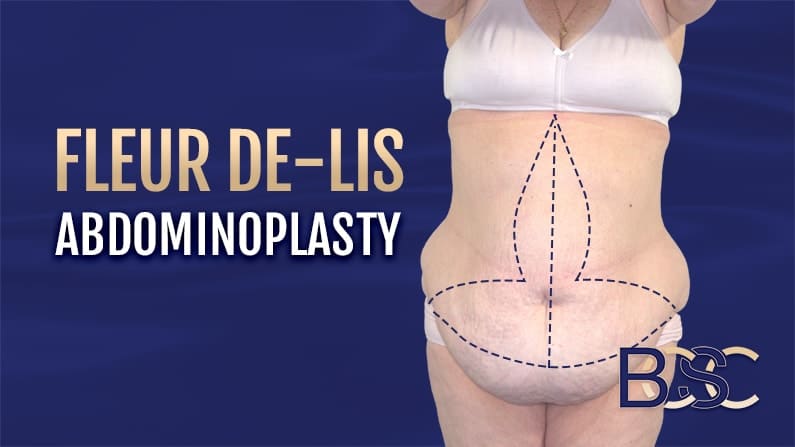
Fleur-de-Lis Abdominoplasty also known as vertical abdominoplasty, is an invasive surgery designed to remove excess skin and fat tissue in the belly region, both horizontally and vertically, after gastric bypass surgery or weight loss.
A study notes, “[f]leur-de-lis abdominoplasty is an effective procedure for correcting abdominal contour abnormalities in both the vertical and horizontal orientation.” Another study on the procedure’s effectiveness notes, “[v]ertical abdominoplasty is an effective procedure to correct abdominal contour abnormalities in individuals with excessive soft tissue in both the vertical and transverse orientation.”

Fleur de lis pattern
The name Fleur-de-Lis in French means “flower of the lily,” which originates from the procedure’s unique incision pattern, which resembles the Iris flower when partially closed. Due to its extensiveness, Fleur-de-Lis abdominoplasty is most suitable for massive weight loss patients with redundant skin on the upper and lower abdomen. However, Fleur-de-Lis is not a weight loss replacement; patients should only consider once weight loss goals have been accomplished and excess skin and fat have been left behind.

Excess skin to remove | BCSC
Fleur de Lis Abdominoplasty Incisions
Fleur de Lis Tummy Tuck (Abdominoplasty) Incisions | BCSC
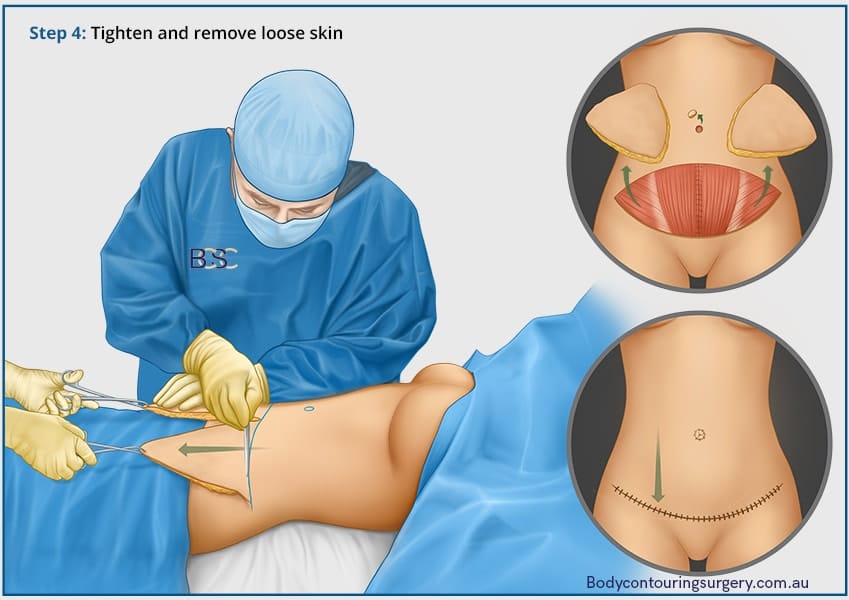
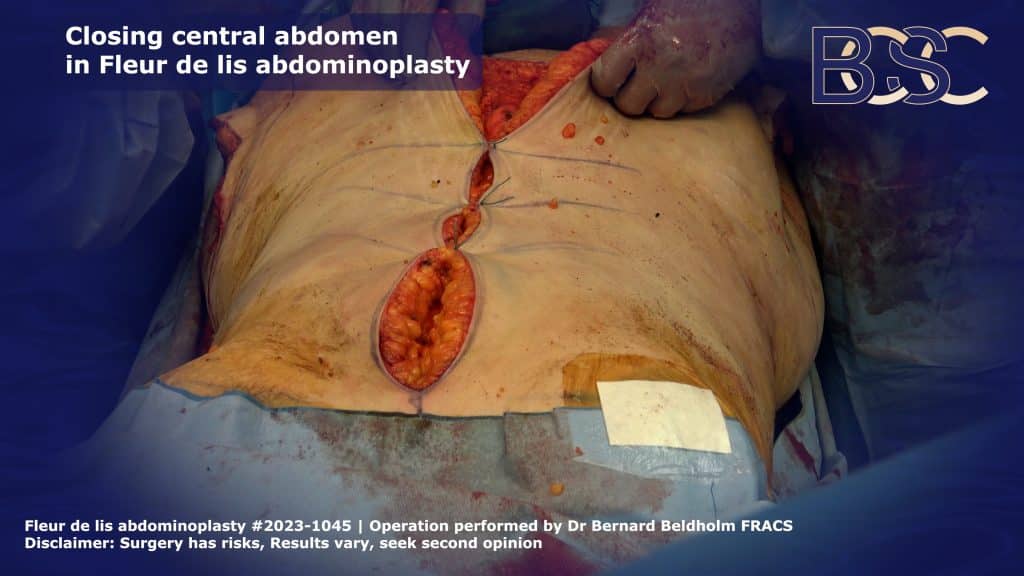
A major surgery, fleur-de-Lis abdominoplasty comprises two incisions; horizontal and vertical. The horizontal incision runs from hip to hip, similar to a traditional abdominoplasty incision. However, unlike traditional abdominoplasty procedures, Fleur-de-Lis has an additional vertical scar running from the pubis to above the belly button, just below the ribs. These incisions allow the specialist surgeon to remove significant skin and fatty tissue in the upper and lower abdomen. When closed, these two incisions form an inverted T shape.
Horizontal Incision
Lower abdominal incision lines | Dr Beldholm
The horizontal incision is similar to a standard abdominoplasty. It runs horizontally along the waistline (hip-to-hip). The horizontal incision targets excess skin tightening on the lower abdominal wall, with its length depending on the amount of loose skin. Dr. Beldholm determines this through the “pinch method,” where he pinches the loose skin to determine the amount to remove.
Vertical Incision
Vertical incision of a fleur de lis abdominoplasty | BCSC
The vertical incision extends from the pubis and runs along the midline, which is the procedure’s defining incision. Similar to the horizontal incision, the vertical incision length depends on the amount of skin the specialist surgeon removes. Commonly, the two length types depend on whether the incision begins below or above the belly button.

Before and after fleur de lis abdominoplasty
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Potential Scar-Related Risks
Scarring is normal after surgery, with the scars fading with time and becoming less noticeable. However, there are instances when a patient develops abnormal scars. A study on scarring following a weight loss surgery notes that “[u]nfavourable scarring is not uncommon following cosmetic surgery; the incidence can vary from 5% after breast augmentation to as high as 8% after tummy tuck (abdominoplasty) procedure.” The study also notes the causes of poor scarring. “[p]postoperative infection, wound dehiscence, tissue necrosis, or simply from abnormal healing tendencies.”
The effects of abnormal scarring can be devastating for the patient, ranging from physical and psychological distress to financial hardships due to the high cost of scar treatment options.
Therefore, minimising the risk of excess scarring after Fleur-de-Lis abdominoplasty should be prioritised. However, patients should understand that minimising the risk of excess scaring involves both the surgeon’s expertise and the patient’s adherence to post-operative instructions.
Possible complications after FDL surgery
Abnormal Scars After FDL Surgery
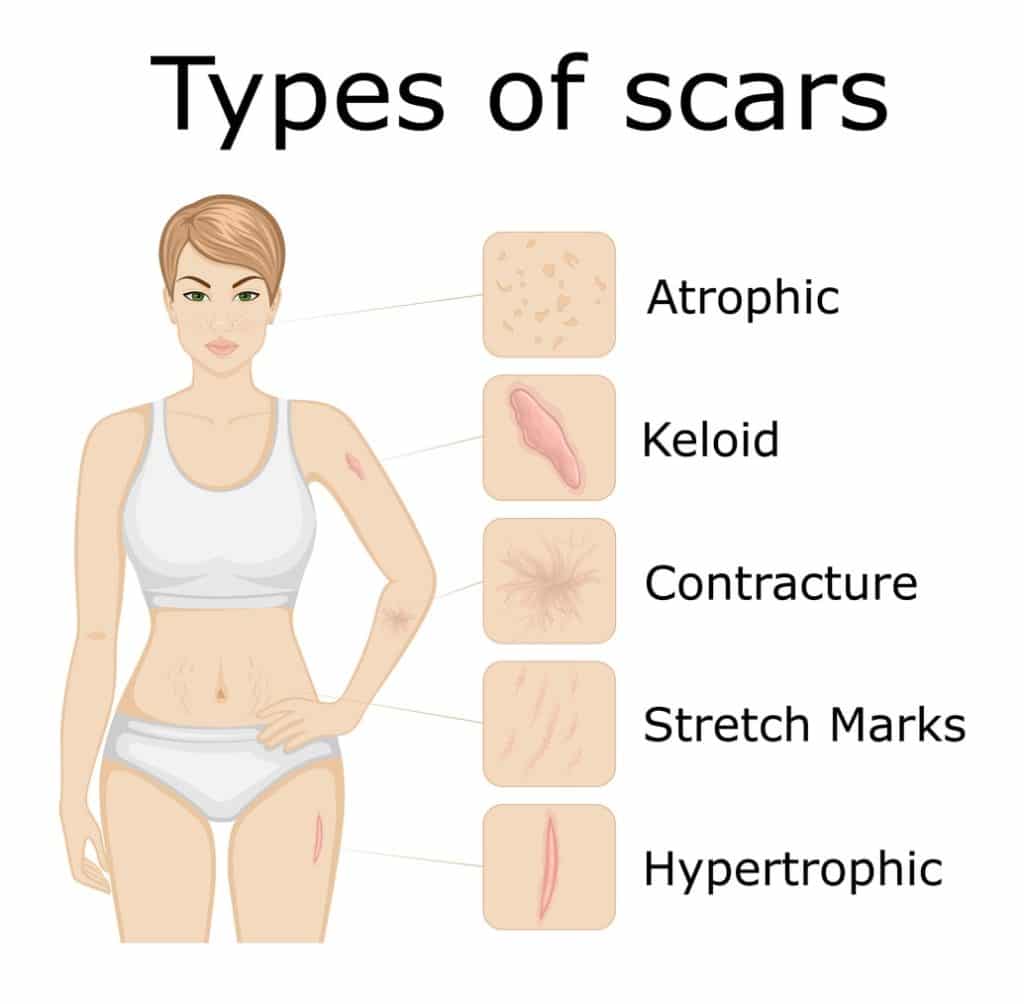
Hypertrophic Scarring
Hypertrophic scars are thick, wide, raised, mostly pink or red scars that develop at the incision site. These types of scars often result from increased amounts of collagen around the region due to increased tension on the wound. Collagen is a connective tissue produced by the body to repair the skin tissue after damage. Increased amounts of collagen will often result in such raised scars, which are easily noticeable.
The most common causes of hypertrophic scarring are hypertension and systemic inflammation. A study on hypertrophic scars notes, “Hypertrophic scars and keloid scars often develop on areas of the body that undergo the most skin tension. These include the back, chest, and upper arms, or the occurrence of any scar over a bony or soft-tissue prominence.”
Hypertrophic scars are unlikely to develop in regions with minimal skin tension.
Keloid Formation

Keloids are wide, raised, ridged, hairless scars, mostly purple or red, which are severe manifestations of hypertrophic scars. These scars spread past the incision site, unlike hypertrophic scars.
Keloids, like hypertrophic scars, mainly develop in areas likely to experience excess skin tension, including the chest, upper abdomen, upper arms, and back, or on bony regions with soft-tissue prominence. Additionally, keloid lesions can develop as early as 1 to 3 months or even as late as one year after surgery.
Scar Dehiscence

Scar dehiscence, also known as wound breakdown or wound separation, is a condition where the wound re-opens due to excess pressure on the sutures, wound infection, poor suturing, or decreased blood flow to the wound. Therefore, it’s important to avoid exerting excess pressure on the wound and ensure it is clean and bacteria-free.
Infection
Scar infection is a common complication after abdominoplasty, mainly caused by a bacterial infection on the wound. Ideally, infections are among the top five most common complications after abdominoplasty, occurring in 1% to 3.8% of cases, including operative site infection and infected seromas.
Infections on the scar are often characterised by erythema (abnormal redness), soreness, tenderness, oedema, and increased temperatures.
Pigmentation Changes

The scar pigmentation may change during scar maturation; hence, the patient may develop hyperpigmented or hypopigmented scars. Pigmentation problems result from other skin trauma, deep partial-and-full thickness burns, and surgical procedures.
Hypopigmentation is when the scar appears lighter than the adjacent skin due to less melanin on the scar, hence appearing as whitish and pale. One of the major signs of hypopigmentation is skin that is lighter than the rest of the skin’s individual colour, though it does not completely lack pigment.

On the other hand, hyperpigmentation is a condition in which the scar appears darker than the adjacent skin. This results from abnormal release of melanin or hyperpigmentation in the dermis and/or epidermis in response to either exogenous or endogenous inflammatory conditions.
Contracture
Contracture is common in patients with a minimal fat layer between the muscle and the dermis layer of the skin. This causes the scar to attach to the muscle layer, making it appear stretched and pulled. These types of scars are also known as tethered scars and mainly occur if the body fails to repair the excess tissue under the wound.
Asymmetry
Asymmetry occurs when the scar doesn’t look symmetrical or appears crooked. Scar asymmetry, is one of the causes of patient dissatisfaction after abdominoplasty surgery. A study on scar asymmetry notes that “[s]car asymmetry after abdominoplasty has been rarely considered a complication.
Scar asymmetry may occur due to an asymmetrical incision during surgery or from complications like chronic seroma.
Wound Healing Complications
Wound healing after FDL Abdominoplasty surgery undergoes the same stages as other wounds. However, it may experience more complications due to increased trauma on the skin. Therefore, the patient and the surgeon should take optimum care to reduce these potential complications. These complications include umbilicus necrosis, skin necrosis, dog ears, poor wound healing process, haematoma, and seroma, among other complications.
Dr Bernard Beldholm | surgery after significant weight loss
How to reduce the Risk of Outer Scars After Fleur-de-Lis (FDL) Abdominoplasty
Reducing the risk of outer scars after Fleur-de-Lis (FDL) Abdominoplasty should be a top priority. The effectiveness ranges from preoperative preparation to postoperative care and treatments. A research study notes, “[t]he challenge is to make scars as inconspicuous as possible, and there are many techniques to be considered, including proper patient selection, preoperative preparation, the choice of surgical techniques, and postoperative care.”
Let’s look at the key ways to reduce the risk of outer scars after Fleur-de-Lis Abdominoplasty;
Post-Operative Care
After surgery, the surgeon will provide you with a list of instructions to reduce the risk of abnormal scarring. Be sure to follow these instructions and contact your specialist surgeon if you notice anything peculiar. Follow these postoperative care instructions:
- Avoiding smoking (at least 6 weeks before and after surgery).
- Follow wound care instructions.
- Wear support garments.
- Avoid strain on the incision.
- Wear loose clothing.
- Stay hydrated and maintain a healthy diet.
- Protect the incision from excess sunlight.
- Attend all follow-up appointments.
Adjunctive Treatments
- Silicone Sheets or Gels: This mode of treatment uses “self-adhesive medical silicone sheets” that protect the skin and aid in moisture retention and balance. By enhancing skin hydration, scar healing is optimised and excess scarring and scar visibility is minimised.
- Scar Massage: Massaging the scar helps promote blood circulation around the region and aids in the realignment of the collagen fibres. This reduces the scar’s rigidity and reduces abnormal scarring. However, patients should take care not to injure the wound during the process.
- Compression Garments: Compression garments apply pressure to the incision site. The pressure helps reduce swelling and bruising, and promotes blood circulation, enhancing scar healing. It also aids in ensuring tissue alignment. Dr Bernard recommends wearing a compression garment for at least six weeks after Fleur-de-Lis Abdominoplasty.
- Topical Treatments: Some common topical scar treatments include antibiotic ointment, petroleum jelly, cocoa butter, vitamin D, scar cream, and vitamin E. These treatments are primarily applied on the skin surface to moisturise the skin and soften the scars.
Medical Interventions
- Steroid Injections: These injections help minimise the appearance of raised, thick abdominoplasty scars. The surgeon injects the steroids directly onto the scar immediately after surgery to prevent abnormal scarring or a few weeks after surgery to correct abnormal scarring.
- Laser Therapy: This treatment uses lasers to penetrate the skin. Laser therapy helps prevent and correct raised scars and reduce scar itch and pain.
- Microneedling: The treatment involves making tiny holes in the skin using sterile, tiny needles. This promotes collagen production, enhancing scar healing and reducing scar visibility. Microneedling is also known as “collagen induction therapy.”
- Pressure Therapy: Pressure therapy involves using garments that induce pressure on the incision region. Pressure therapy helps limit fibroblast activity, thus reducing the risk of excess scarring.

Dr. Bernard Beldolm’s Advice on Outer Scar Following FDL Surgery
Scarring after Fleur-de-Lis (FDL) Abdominoplasty is normal. However, excess scarring is not, and can have physical and physiological effects. Some common abnormal scarring after Fleur-de-Lis Abdominoplasty include keloids, hypertrophic, and hypo or hyperpigmented scars.
Therefore, taking precautions to reduce the risk of outer scars following Fleur-de-Lis Abdominoplasty, ranging from preoperative to postoperative preparation, is important.
References
- Mitchell, R. T., & Rubin, J. P. (2014). The Fleur-De-Lis abdominoplasty. Clinics in plastic surgery, 41(4), 673–680.
- Friedman, T., O’Brien Coon, D., Michaels V, J., Purnell, C., Hur, S., Harris, D. N., & Rubin, J. P. (2010). Fleur-de-Lis abdominoplasty: a safe alternative to traditional abdominoplasty for the massive weight loss patient. Plastic and reconstructive surgery, 125(5), 1525–1535.
- Cannistrà, C., Lori, E., Arapis, K., Gallo, G., Varanese, M., Pironi, D., De Luca, A., Frusone, F., Amabile, M. I., Sorrenti, S., Gagliardi, F., & Tripodi, D. (2024). Abdominoplasty after massive weight loss. Safety preservation fascia technique and clinical outcomes in a large single series-comparative study. Frontiers in surgery, 11, 1337948.
- Chambers, A. (2020). Management of scarring following aesthetic surgery. In Springer eBooks (pp. 385–395).
- Schmieder, S. J., & Ferrer-Bruker, S. J. (2023, September 4). Hypertrophic scarring. StatPearls – NCBI Bookshelf.
- Vidal, P., Berner, J. E., & Will, P. A. (2017). Managing Complications in Abdominoplasty: A Literature Review. Archives of plastic surgery, 44(5), 457–468.
- Pijpe, A., Gardien, K. L. M., Van Meijeren-Hoogendoorn, R. E., Middelkoop, E., & Van
- Zuijlen, P. P. M. (2020). Scar symptoms: pigmentation disorders. In Springer eBooks (pp. 109–115).
- Mendes, F. H., Donnabella, A., & Fagotti Moreira, A. R. (2019). Fleur-de-lis Abdominoplasty and Neo-umbilicus. Clinics in plastic surgery, 46(1), 49–60.
- Ziegler, U. E., Ziegler, S. N., & Zeplin, P. H. (2017). Modified Fleur-de-lis Abdominoplasty for Massive Weight Loss Patients. Annals of plastic surgery, 79(2), 130–134.
- Dellon, A. L. (1985c). Fleur-de-lis abdominoplasty. Aesthetic Plastic Surgery, 9(1), 27–32.
- Di Summa, P. G., Wettstein, R., Erba, P., Raffoul, W., & Kalbermatten, D. F. (2013). Scar asymmetry after abdominoplasty. Annals of Plastic Surgery, 71(5), 461–463.
- De Decker, I., Beeckman, A., Hoeksema, H., De Mey, K., Verbelen, J., De Coninck, P., Blondeel, P., Speeckaert, M. M., Monstrey, S., & Claes, K. E. Y. (2023). Pressure therapy for scars: Myth or reality? A systematic review. Burns : journal of the International Society for Burn Injuries, 49(4), 741–756.
- Van Den Kerckhove, E., & Anthonissen, M. (2020). Compression therapy and conservative strategies in scar management after burn injury. In Springer eBooks (pp. 227–231).