Brachioplasty (Arm Lift) After Bariatric Surgery and Extreme Weight Loss
Bariatric surgery or significant lifestyle changes can lead to dramatic weight loss. While this achievement improves health and quality of life, it often leaves behind loose, redundant skin that does not retract naturally. The upper arms are one of the most common areas affected.
For some patients, the excess is limited to the inner upper arms. For others — especially those who have lost more than 40–50 kilograms — redundant skin extends into the axilla (armpit) and down the lateral chest wall. In these cases, extended brachioplasty (arm lift) is often required rather than a standard procedure.
What Is Brachioplasty (Arm Lift)?
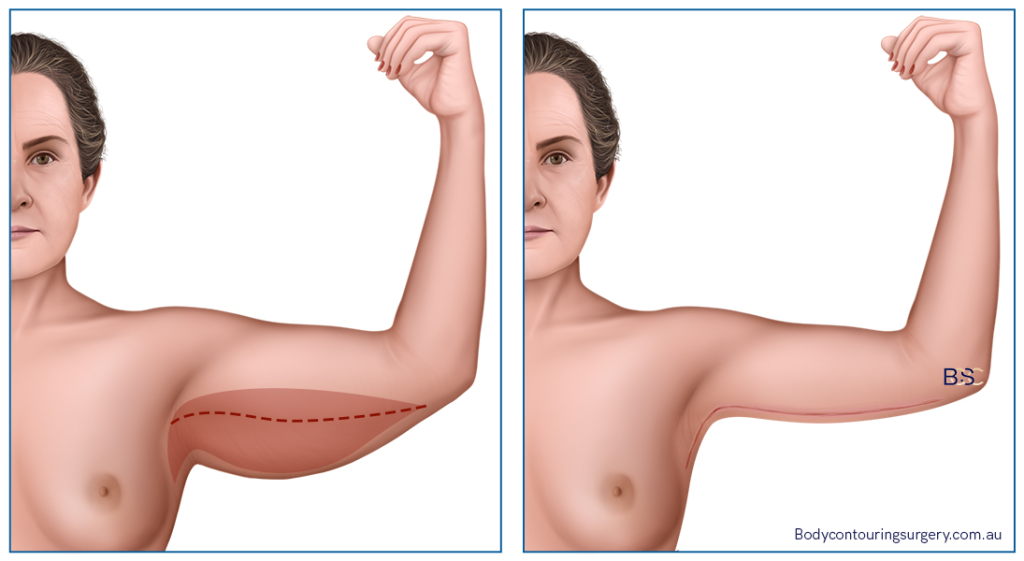
Brachioplasty is a surgical operation designed to remove excess skin and, in selected cases, residual fat from the upper arms. For patients after massive weight loss, it is more than a cosmetic procedure. Redundant skin can cause:
- Recurrent rashes and infections in skin folds
- Difficulty with clothing fit
- Discomfort during exercise
- Social and emotional self-consciousness
In patients with ageing-related laxity, the issue is usually confined to the arms themselves. In contrast, after massive weight loss the skin has been stretched for years and then rapidly deflates, leaving folds across the arms, axilla, and chest wall.
Extended Brachioplasty for Post-Weight Loss Patients
Incision Placement
A standard brachioplasty involves an incision from the elbow to the axilla. Extended brachioplasty continues beyond the axilla and onto the lateral chest wall, addressing the broader areas of skin redundancy.
Anatomical Considerations
Studies have shown that the posterior axillary fold originates from the lateral chest wall (Ref 2). This explains why significant weight changes produce redundant tissue not only in the upper arm but also across the axilla and chest. A short incision cannot adequately correct these changes.
Benefits Beyond Appearance
Extended brachioplasty can improve mobility when large folds interfere with arm movement, reduce chafing and rashes in the axilla, and allow more comfortable clothing fit.
The Role of Suction-Assisted Lipectomy (Liposuction)
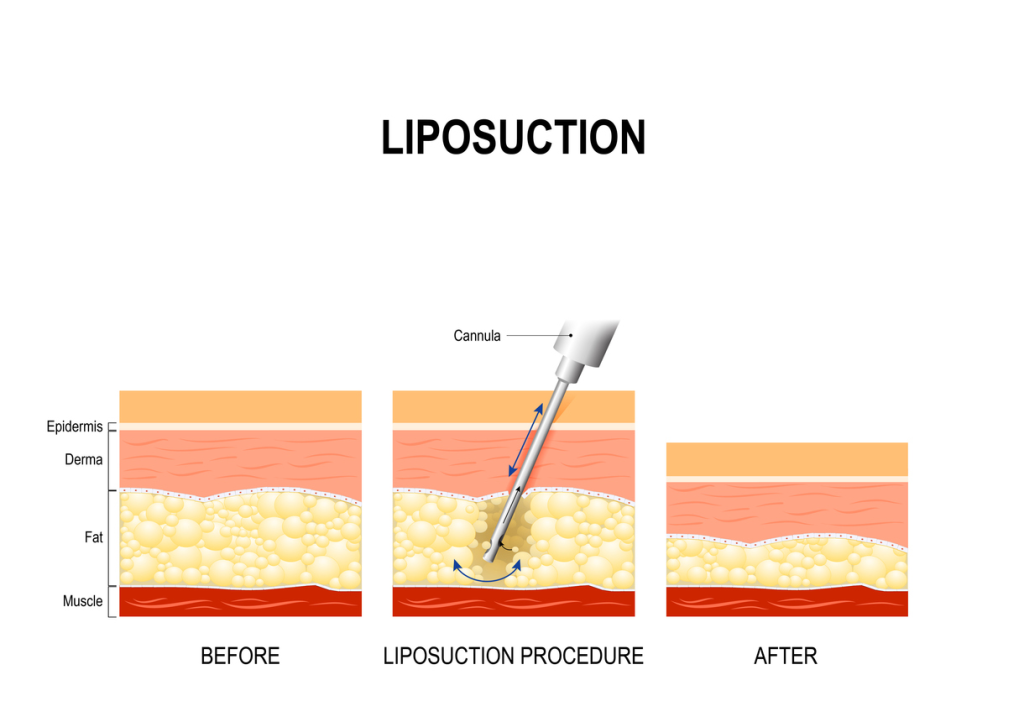
Suction-assisted lipectomy (liposuction) may be performed together with brachioplasty to refine the result. Some post-bariatric patients have residual fat pockets that persist despite major weight loss.
- Technique: The surgeon uses suction-assisted lipectomy to reduce fatty tissue before excising the redundant skin.
- Medical Evidence: A 2018 study (Ref 1) reported that liposuction-assisted brachioplasty preserved vascular, lymphatic, and nervous structures while reducing complication rates. Patients in the study had fewer hypertrophic and keloid scars compared with excision alone.
- Practical Benefits: It can reduce wound tension, improve healing, and provide smoother shaping of the arms and chest wall.
Who Is an Ideal Candidate?
Extended brachioplasty is generally appropriate for patients who:
- Have lost a large amount of weight through bariatric surgery (e.g. gastric bypass, sleeve gastrectomy) or lifestyle changes
- Have redundant skin of the upper arms, axilla, and lateral chest wall
- Have reached a stable weight and maintain a healthy body mass index (BMI)
- Are non-smokers or willing to cease smoking to support wound healing
- Are otherwise in good health to undergo surgery and recovery
Patients with mild laxity from ageing or small weight fluctuations may be better suited to other techniques.
Additional Body Contouring Surgery After Massive Weight Loss
Most post-weight loss patients have redundant skin in multiple body regions. Extended brachioplasty is often part of a staged plan that may also include:
Abdominoplasty (Tummy Tuck)
Removes redundant abdominal skin. In post-bariatric patients, a fleur-de-lis abdominoplasty with both horizontal and vertical incisions may be required.
Belt Lipectomy (Lower Body Lift)
Addresses circumferential laxity around the waistline, improving the abdomen, flanks, buttocks, and outer thighs.
Thighplasty (Thigh Lift)
Removes redundant skin from the thighs, often performed after a belt lipectomy for optimal results.
Breast Surgery After Weight Loss
- Mastopexy (Breast Lift): Elevates and reshapes deflated breasts.
- Reduction Mammoplasty (Breast Reduction): Reduces volume in women with large, heavy breasts.
- Augmentation Mammoplasty (Breast Augmentation): Restores volume with implants in cases of significant deflation.
- Gynaecomastia Surgery: Removes redundant skin and tissue from the male chest.
Suction-Assisted Lipectomy (Liposuction)
Can be added to many body contouring procedures to refine results by targeting stubborn fat pockets.
Risks and Recovery
Like all surgical operations, extended brachioplasty carries risks. These may include:
- Wound-healing difficulties
- Seroma (fluid collection)
- Infection
- Altered or reduced sensation in the arms
- Asymmetry between arms
- Hypertrophic or widened scarring
Recovery varies depending on the extent of surgery and whether additional procedures are performed. Most patients return to light daily activity in 2–3 weeks. Full recovery may take several months, during which compression garments and close follow-up with the surgeon are essential.
Final Thoughts
Extended brachioplasty (arm lift) is often the most effective option for addressing redundant skin in the arms, axilla, and chest wall after bariatric surgery or extreme weight loss. When combined with suction-assisted lipectomy (liposuction), it can provide safer outcomes with improved shaping.
However, it is a significant operation that requires careful planning and a realistic understanding of risks and recovery. A consultation with a qualified specialist surgeon is the best way to determine suitability.
References
- Di Pietro V, Colicchia GM, Cervelli V, Gentile P. Arm Contouring After Massive Weight Loss: Liposuction-Assisted Brachioplasty Versus Standard Technique. Journal of Cutaneous and Aesthetic Surgery. 2018;11(2):73-78.
- Aly A, Pace D, Cram A. Brachioplasty in the patient with massive weight loss. Aesthetic Surgery Journal. 2006;26(1):76-84.