7 Rules to Help Reduce Swelling After Abdominoplasty Surgery
Swelling is a normal and expected part of recovery after abdominoplasty (tummy tuck) surgery. It usually affects not only the incision line but also the entire abdominal region. If liposuction is performed at the same time, swelling may be more noticeable.
While swelling can be uncomfortable, there are evidence-based strategies that can support your healing and help manage it effectively.
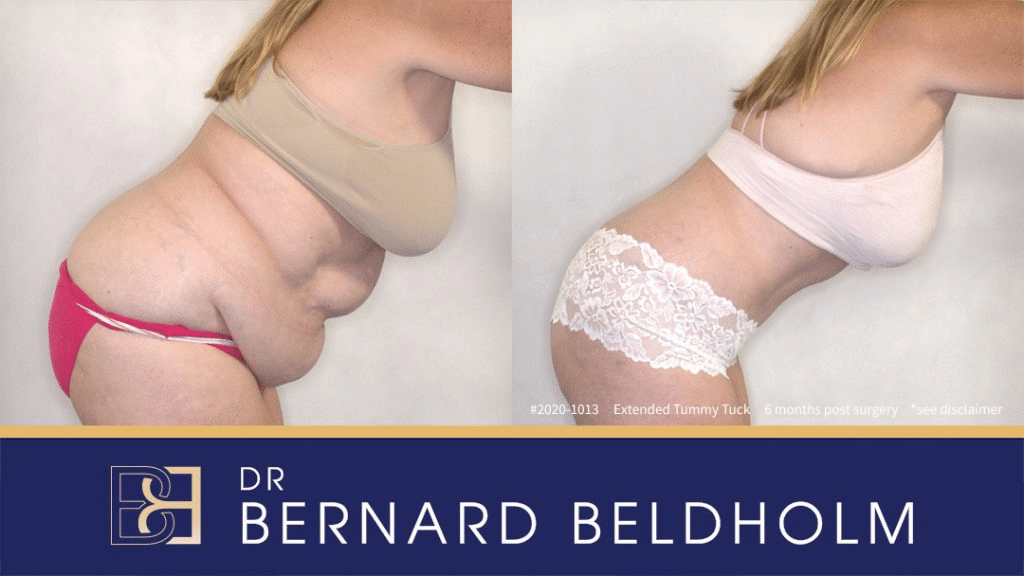
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Why Does Swelling Occur After Abdominoplasty?
Swelling is part of the body’s natural healing response. It occurs as tissues repair and recover following surgery. Common reasons include:
- Normal post-surgical inflammation
After surgery, the body activates its healing response. Specialised cells move to the area to repair tissue, which naturally causes swelling. - Bruising
Some small blood vessels may be affected during surgery. When blood leaks into the surrounding tissues, this can cause bruising and contribute to swelling. - Temporary impact on the lymphatic system
The lymphatic vessels help drain excess fluid from tissues. If they are affected during surgery, fluid may build up, leading to swelling. The body usually adapts over time.
Lymphatic massage can sometimes be used in the early recovery phase to help support fluid drainage, though this should only be performed if recommended by your surgeon.
How Long Does Swelling Last?
- Swelling is most noticeable in the first few weeks after surgery.
- Around 60% of swelling reduces by 3 months.
- At 6 months, about 80% of swelling has usually resolved.
- Residual swelling can continue to settle between 12–18 months.
Most patients find swelling is more prominent in the lower abdomen.
7 Strategies to Help Manage Swelling After Abdominoplasty
1. Prioritise Rest
Adequate sleep gives your body time to repair and regenerate. Growth hormones released during deep sleep play a key role in tissue healing. Poor rest can slow the recovery process.
While rest is important, it is also essential to maintain gentle mobility (see point 2).
2. Incorporate Gentle Movement
Specialist surgeons often recommend light walking soon after surgery. Short walks around the house can:
- Support blood circulation
- Lower the risk of blood clots
- Help reduce swelling
Avoid strenuous exercise or lifting heavy objects until cleared by your surgeon. Elevating your legs while lying down may also help reduce fluid build-up in the lower body.
3. Limit Sodium (Salt) Intake
Excess sodium in the diet can cause water retention and bloating. Reducing salt intake supports healing and may help reduce abdominal swelling. Choose fresh, unprocessed foods and season meals lightly.
4. Wear Your Compression Garment
A medical-grade compression garment applies gentle, even pressure to the surgical area, which can:
- Reduce swelling and bruising
- Support wound healing
- Provide comfort
- Assist with skin retraction in some cases
Most patients are advised to wear their garment for at least 4–6 weeks, although some may need longer depending on the extent of surgery. Always follow your surgeon’s specific instructions.
5. Maintain a Healthy Diet and Stay Hydrated
A balanced diet provides the nutrients needed for tissue repair. Key elements include:
- Protein – for wound healing and scar repair
- Vitamins A & C, zinc and iron – to support immune function and recovery
- Whole grains, vegetables, and lean proteins – for sustained energy
Staying well hydrated is equally important. Adequate water intake helps blood deliver oxygen and nutrients to the surgical site. Dehydration may slow recovery and prolong swelling.
6. Take Medication Only as Prescribed
Anti-inflammatory medications may be recommended to help with pain and swelling. However, some medicines can increase bleeding risk if taken too early. Only use the medications prescribed or approved by your surgeon, and never self-medicate without guidance.
7. Consider Lymphatic Massage (If Recommended)
Lymphatic drainage massage is a specialised technique designed to encourage fluid movement in the tissues. When appropriate, your surgeon may suggest this as part of your recovery plan. It should only be performed by a trained professional and under your surgeon’s guidance.
Follow-Up Care is Essential
Attending your scheduled post-operative appointments allows your surgeon to:
- Monitor your healing
- Adjust your care plan if needed
- Provide advice on garment wear and activity levels
- Address any concerns you may have
Always follow your surgeon’s instructions closely, as every patient’s recovery journey is unique.
Key Takeaway
Swelling after abdominoplasty (tummy tuck) is a normal part of recovery. While it cannot be completely avoided, these seven strategies can support healing and help reduce discomfort over time. With rest, good nutrition, appropriate activity, and ongoing follow-up care, swelling usually improves gradually in the months after surgery.
References
- Elkhenany, H., AlOkda, A., El-Badawy, A., & El-Badri, N. (2018). Tissue regeneration: Impact of sleep on stem cell regenerative capacity. Life Sciences, 214, 51–61.
- Vidal, P., Berner, J. E., & Will, P. (2017b). Managing Complications in Abdominoplasty: A Literature review. Archives of Plastic Surgery, 44(05), 457–468.
- Najera, R. M., Asheld, W. J., Sayeed, S. M., & Glickman, L. T. (2011). Comparison of Seroma Formation following Abdominoplasty with or without Liposuction. Plastic and Reconstructive Surgery, 127(1), 417–422.
- Hardy, K. L., Davis, K. E., Constantine, R. S., Chen, M., Hein, R. E., Jewell, J. L., Dirisala, K., Lysikowski, J., Reed, G., & Kenkel, J. M. (2014). The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. Aesthetic Surgery Journal, 34(4), 614–622.
- Rangaswamy, M. (2013). Minimising complications in abdominoplasty: An approach based on the root cause analysis and focused preventive steps. Indian Journal of Plastic Surgery, 46(2), 365.
- Dixit, V., & Wagh, M. S. (2013). Unfavourable outcomes of liposuction and their management. Indian Journal of Plastic Surgery, 46(2), 377.
- Fogacci, T., Cattin, F., Semprini, G., Frisoni, G., Fabiocchi, L., & Samorani, D. (2019). The negative pressure therapy with PICO as a prevention of surgical site infection in high‐risk patients undergoing breast surgery. Breast Journal, 26(5), 1071–1073.
- De Moraes, B. Z. F., Ferreira, L. M., Martins, M. R. C., Rostom, L., De Castro, H. a. S., & Nahas, F. X. (2022). Do compression garments prevent subcutaneous edema after abdominoplasty? Aesthetic Surgery Journal, 43(3), 329–336.
- Kosloski, F. R., Barbosa, M. V. J., Rodrigues, M. A., Martins, M. R. C., Ferreira, L. M., & Nahas, F. X. (2023). Effect of compression garments on the ventilatory function after abdominoplasty. Aesthetic Surgery Journal.
- Bray, G. A., & Ryan, D. H. (2020). Evidence‐based weight loss interventions: Individualized treatment options to maximize patient outcomes. Diabetes, Obesity and Metabolism, 23(S1), 50–62.
- Harris, L., & Darby, P. (2020a). Enhanced Recovery after Abdominoplasty Using Perisurgical Nutritional Supplementation. Plastic and Reconstructive Surgery. Global Open, 8(12), e3314.
- Rangaswamy, M. (2013b). Minimising complications in abdominoplasty: An approach based on the root cause analysis and focused preventive steps. Indian Journal of Plastic Surgery, 46(2), 365.
- Coppa, K., Kim, Y. H., Oppenheim, M., Bock, K., Conigliaro, J., & Hirsch, J. S. (2021). Examination of post-discharge follow-up appointment status and 30-Day readmission. Journal of General Internal Medicine, 36(5), 1214–1221.