Popular Weight Loss Medications vs Bariatric Surgery
When it comes to managing obesity, both weight loss medications and bariatric surgeries remain popular, though distinct options for individuals struggling to lose weight with diet and exercise alone. With each involving its own set of risks, benefits, and lifestyle considerations, choosing between these options depends on many factors, including cost, personal commitments and responsibilities, health status, weight loss goals, and willingness to commit to lifestyle changes.
Weight loss medications affect one’s appetite, metabolism, or fat absorption, offering a non-invasive solution that supports gradual weight loss in the short-term. Weight loss surgery, on the other hand, involves more invasiveness, yielding long-lasting permanent changes to the digestive system. By limiting food intake or absorption, bariatric surgery offers patient long-lasting and significant weight loss.
Because each approach comes with its own set of benefits, risks, and considerations, it is crucial for individuals to understand the differences and determine the most appropriate treatment. In this article, we’ll explore the key aspects of weight loss medications and bariatric surgery to clarify their roles in the fight against obesity.

Doctor reviewing health history with patient
Dangers of Obesity in Adults
Obesity in adults carries a range of serious medical conditions and health risks that can significantly impact quality of life and lead to life-threatening obesity related diseases. Some of the most common dangers include:
- Heart Disease: Obesity increases the risk of high blood pressure, high cholesterol, and atherosclerosis, which can lead to heart attacks, strokes, and heart failure.
- Type 2 Diabetes: Excess weight may contribute to insulin resistance, making it more difficult for the body to regulate blood sugar levels, often leading to type 2 diabetes.
- Sleep Apnea: Obesity is a major risk factor for sleep apnea, a condition where the airway becomes blocked during sleep, causing breathing interruptions and poor sleep quality.
- Joint Problems: Carrying excess weight puts additional strain on joints, especially the knees, hips, and lower back, leading to conditions like osteoarthritis.
- Cancer: Obesity is linked to an increased risk of certain types of cancer, including breast, colon, and kidney.
- Fatty Liver Disease: Non-alcoholic fatty liver disease (NAFLD) is more common in obese individuals, which can lead to liver inflammation, scarring, and even liver failure.
- Mental Health Issues: Obesity can contribute to depression, anxiety, and low ** due to body image concerns and social stigma.
- Respiratory Problems: Obesity can impair lung function and contribute to respiratory problems, such as asthma and shortness of breath.
These health risks highlight the importance of managing obesity through a combination of lifestyle changes, medical interventions, and, in some cases, surgery or medications to reduce the likelihood of developing serious, long-term health problems.

BMI for determining bariatric procedures or weight loss injection eligibility
Determining your BMI (Body Mass Index)
To determine your BMI (Body Mass Index), you can use a ** formula that takes into account your weight and height.
Formula: BMI = weight (kg) / height (m)²
Once calculated, you can compare your result to standard BMI categories: underweight (less than 18.5), normal weight (18.5-24.9), overweight (25-29.9), and obese (30 or higher). There are also many online calculators that can ** calculate your BMI for you.
Weight Loss Medications

Weight loss medications
Weight loss medications such as Injectable GLP-1 Agonists are designed for individuals who are overweight or obese and have failed to lose weight through traditional methods like diet and exercise. Medications help by reducing the appetite and increasing satiety.
How Weight Loss Injections Work
Weight loss injections primarily work by affecting hormones that control hunger and satiety. For example, semaglutide mimics a hormone called GLP-1, which helps regulate appetite and insulin levels. These medications may help you feel fuller for longer, reduce cravings, and ** the body’s ability to burn fat, leading to weight loss when combined with a healthy diet and exercise.

Injectable GLP-1 Agonists
Injectable GLP-1 Agonists
Indications/Eligibility:
- BMI Over 27
- Best for individuals with moderate obesity or those who have not had success with diet/exercise alone.
Frequency
- Once/Week
Period of Treatment
- Lifelong
Mechanisms of Action
- Induces satiety and slows down stomach contractions
Availability
- Widespread, any doctor can prescribe
TBWL: Total Body Weight Loss %
- 12 – 17%; 20% of patients may lose >20% of TBW but mostly on higher/ maximum dose
TBWL (Total body weight loss %) – Strict research conditions
- 70% Lost >20% of TBW but gained all the weight back in the next 50-60 weeks
TBW % Loss Long Term
- 15% at 10-15 years
Serious side effects/ complications
- 3%
Effects of metabolic syndrome (Diabetes, high cholesterol and related diseases)
- Moderate and recurred once medications were stopped or weight was regained
Recurrence of metabolic syndrome
- Soon after medication was stopped and weight was regained
Cost
- Varies by insurance coverage, concern, condition, source
- Ongoing for life.
- Equals the cost of surgery in 3.5 years (and then still on going)

Pros and cons of weight loss medications
Pros and Cons of Weight Loss Medications
Pros:
- Non-invasive: No surgery required.
- Temporary Solution: Can be part of a larger weight management plan that includes lifestyle changes.
- Variety of Options: Different medications work in different ways (e.g., appetite suppressants, fat absorption blockers, or metabolic **).
- ** for Long-term Use: Can be used for long-term weight management under medical supervision.
Cons:
- Side Effects: Some medications have side effects like nausea, headaches, or increased heart rate.
- Not a permanent solution: Medications must be taken regularly to maintain their effects, and weight often returns once the medication is stopped.
- Not effective for everyone: Some individuals may not respond to medications as expected.
- Need for lifestyle changes: Medications work best when combined with diet and exercise, and they do not replace the need for those.

Diet restrictions while using weight loss medications
Diet Restrictions While Using Weight Loss Medications
When taking weight loss injections like semaglutide, a special diet is not typically required, but it is crucial to follow a healthy eating plan to maximize the effectiveness of the injections and support sustainable weight loss.
These medications help reduce appetite and promote feelings of fullness, but combining them with a balanced diet and regular physical activity will ** results and ** overall health. Here are some general guidelines to follow while using weight loss injections:
1. Focus on Portion Control
- Weight loss injections decrease one’s appetite, so it’s easier to control portion sizes. Eating smaller, balanced meals throughout the day rather than large portions helps prevent overeating and supports your body’s ability to lose weight.
2. Prioritize Nutrient-Dense Foods
- Vegetables: Fill half your plate with non-starchy vegetables, such as leafy greens, broccoli, cauliflower, and bell peppers.
- Protein: Incorporate lean protein sources, such as chicken, turkey, fish, tofu, eggs, and legumes to increase satiety (full feeling) and preserves muscle mass.
- Whole Grains: Choose whole grains like brown rice and oats instead of refined grains.
- Healthy Fats: Include sources of healthy fats like avocado, nuts, seeds, and olive oil.
3. Limit Processed and High-Sugar Foods
- Though the weight loss injections help manage hunger, it’s still important to avoid processed foods, sugary snacks, and beverages which can interfere with weight loss and contribute to health issues like insulin resistance and high blood sugar.
- Reduce the intake of sugary drinks, sweets, baked goods, and fast food, opting for whole, unprocessed foods to help maintain energy levels and promote long-term weight loss.
4. Stay Hydrated
- Drinking plenty of water (at least 8 cups (64 ounces) of water daily depending on your activity level) is essential, as hydration can aid in digestion, support metabolism, and help prevent constipation, which can be a side effect of weight loss injections.
5. Meal Timing and Frequency
- While there’s no one-size-fits-all approach to meal timing, it’s beneficial to eat regular meals and snacks. Though it’s natural to eat fewer meals throughout the day, it’s still important to eat balanced meals to ensure the body receives the nutrients it needs.
6. Exercise and Lifestyle
- A healthy diet is most effective when paired with physical activity (at least 150 minutes of moderate-intensity exercise like walking, swimming, or cycling per week) along with strength training exercises to maintain a healthy muscle mass.
7. Monitor Side Effects
- Weight loss injections may cause some digestive issues, like nausea or constipation, particularly in the first few weeks. Adjusting your diet to include fiber-rich foods (such as whole grains, fruits, and vegetables) can help manage these side effects. Also, eating smaller, more frequent meals can help reduce nausea.

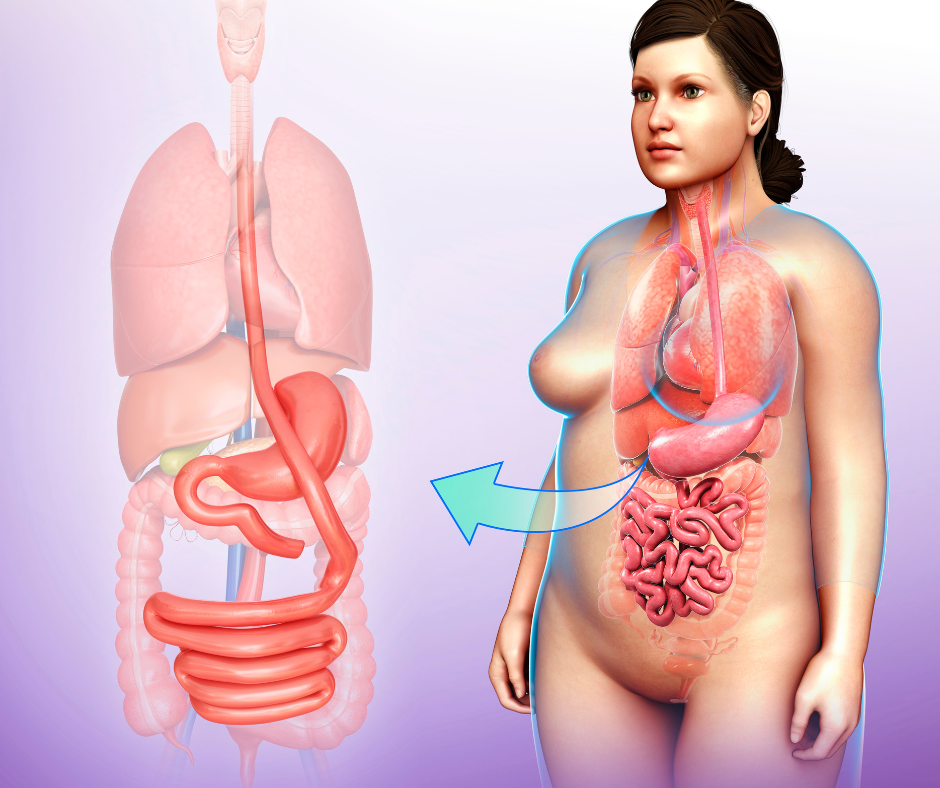
Metabolic and Bariatric Surgery
Weight Loss (Bariatric) Surgery
Bariatric surgery is typically recommended for individuals who are severely obese (usually with a BMI of 35 or higher or a BMI of 30 with obesity-related conditions like diabetes) and who have been unable to lose weight through non-surgical methods.
New stomach pouch
Types of Bariatric Surgery Procedures
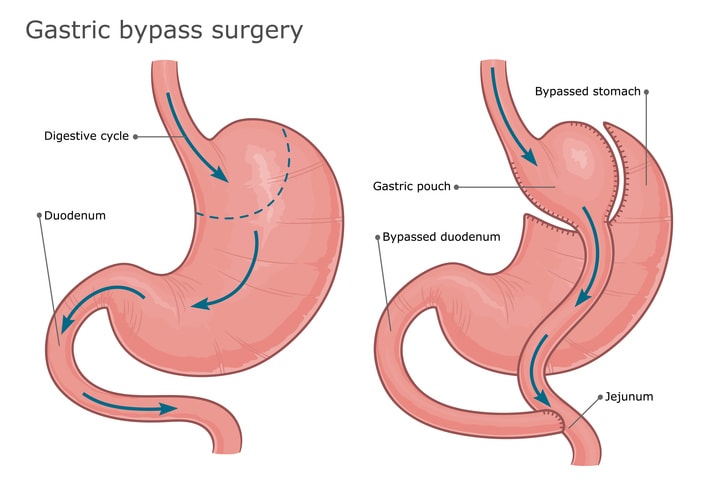
Gastric Bypass Surgery
Gastric bypass surgery
Gastric bypass, which is performed while the patient is under general anesthesia, works by creating a smaller pouch at the top of the stomach, which is then directly connected to the small intestine, bypassing a portion of the stomach and the upper part of the small intestine. This reduces the amount of food the stomach can hold and limits the absorption of calories and nutrients. As a result, patients feel fuller faster and absorb fewer calories, leading to significant weight loss. Subsequently, the surgery may also resolve obesity-related conditions like type 2 diabetes, high blood pressure, and sleep apnea.
Laparoscopic Gastric Bypass Surgery
Gastric bypass surgery can be performed laparoscopically, which is the most common approach today. Laparoscopic gastric bypass involves making several small incisions in the abdomen through which a camera and specialized instruments are inserted to perform the surgery. This minimally invasive technique offers several advantages over traditional open surgery, including smaller incisions, less pain, a shorter recovery time, and a reduced risk of complications such as infections and scarring. Most patients who are candidates for gastric bypass are able to undergo the laparoscopic procedure, as long as there are no contraindications.
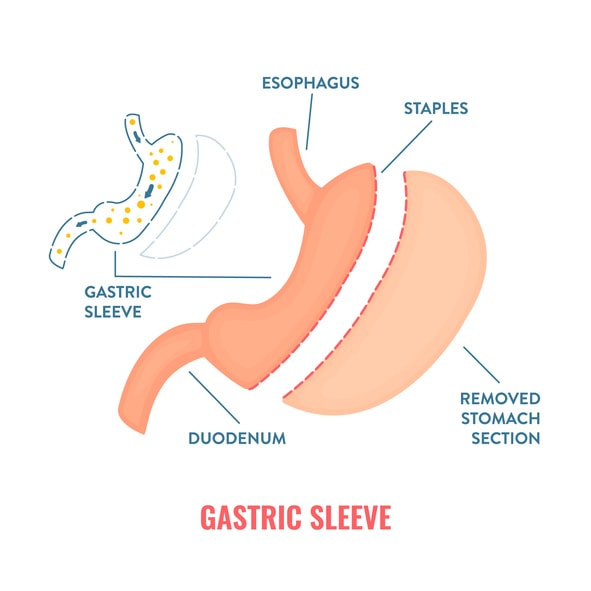
Sleeve Gastrectomy (Vertical Sleeve Gastrectomy)
Sleeve gastrectomy
A relatively ** procedure, sleeve gastrectomy, also known as vertical sleeve gastrectomy, works by removing about 80% of the stomach, leaving a small, banana-shaped “sleeve” or tube. This significantly reduces the stomach’s size and capacity, limiting the amount of food a person can consume at one time.
In addition to restricting food intake, the surgery also alters hunger-regulating hormones, which helps reduce appetite and cravings. As a result, patients typically experience significant weight loss, as they eat less and feel fuller more **. This procedure is less invasive than other types of weight loss surgery and does not involve rerouting the intestines.
Laparoscopic sleeve gastrectomy
Using minimally invasive techniques, laparoscopic sleeve gastrectomy involves removing a large portion of the stomach, leaving a smaller, sleeve-shaped stomach.
About 75-80% of the stomach is removed, leaving a narrow tube or “sleeve,” about the size and shape of a banana. With a smaller stomach, patients can only eat a smaller amount of food, which helps in reducing overall calorie intake. The surgery also impacts hunger-related hormones, especially ghrelin, which is often called the “hunger hormone.” Its levels drop after surgery, reducing appetite.
This procedure is often used for patients who are severely obese and haven’t had success with diet, exercise, or other weight loss procedures.

Smaller stomach
Key Differences Between Sleeve Gastrectomy and Gastric Bypass
- Surgical Complexity: Gastric bypass is more complex and invasive than a sleeve gastrectomy, requiring more extensive changes to both the stomach and intestines.
- Effectiveness for Diabetes: Gastric bypass tends to be more effective for people with type 2 diabetes due to the changes in digestion and absorption.
- Nutrient Absorption: Gastric bypass causes malabsorption, whereas sleeve gastrectomy does not. Therefore, people who undergo gastric bypass often need to take nutritional supplements.
- Weight Loss Speed: Gastric bypass generally results in faster weight loss initially, but both surgeries can lead to significant and sustained weight loss.

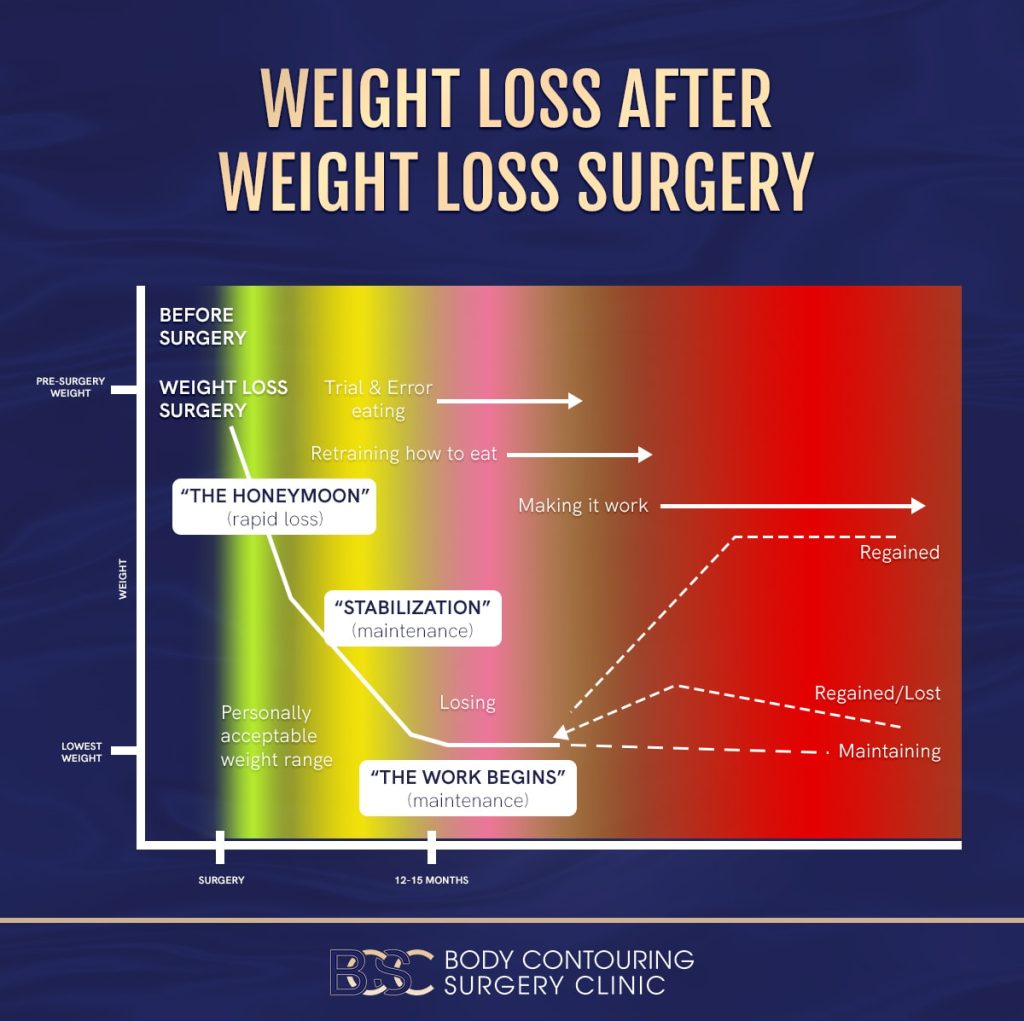
What to expect after weight loss surgery?
What to Expect After Weight Loss Surgery
For patients who have tried to lose weight but failed, Bariatric surgery can lead to significant long-term benefits, thought it also requires lifelong commitment to lifestyle changes and ongoing medical monitoring. Here are the key long-term results that individuals can expect following gastric bypass surgery:
1. Significant Weight Loss
What to expect after weight loss surgery?
- Most people experience substantial weight loss, typically losing 60-80% of their excess body weight within the first 18–24 months. Weight loss generally continues for up to two years, with some people maintaining a stable weight or experiencing gradual weight regain after that.
- The weight loss is generally sustained over the long term, but it may require a continued focus on diet, exercise, and behavior modifications to prevent regain.
2. ** or Resolution of Obesity-Related Conditions
Several obesity related health problems can be resolved with weight loss surgery, including:
- Type 2 Diabetes: Many patients see ** or even complete remission of type 2 diabetes after surgery, often within a few months, as the body’s ability to regulate blood sugar **.
- Sleep Apnea: Significant ** in sleep apnea symptoms, or complete resolution, is common as weight decreases.
- Hypertension: Many individuals experience a reduction in blood pressure, sometimes eliminating the need for medications.
- Joint Pain: Reduced strain on joints and ** in conditions like osteoarthritis are common as patients lose weight.
3. Nutritional Deficiencies
- Since gastric bypass surgery reduces the size of the stomach and bypasses part of the small intestine, nutrient absorption can be impaired. This increases the risk of deficiencies in vitamins and minerals, including vitamin B12, iron, calcium, and vitamin D.
- Lifelong vitamin supplementation and regular blood tests are required to monitor nutrient levels and prevent deficiencies, which can lead to serious health issues if not **.
4. Digestive Issues
- Some people experience dumping syndrome, which occurs when food moves too ** from the stomach into the small intestine. Symptoms can include nausea, vomiting, diarrhea, and dizziness, especially after eating sugary or high-fat foods.
- Other digestive problems can include bloating, gas, and changes in bowel movements, especially during the first year after surgery.
5. Psychological and Emotional Impact
- Many people experience ** mental health and quality of life due to the physical and emotional benefits of significant weight loss.
- However, the psychological impact of the changes in body image and the need for ongoing lifestyle changes can also pose challenges. Support groups or counseling can be helpful for ** any emotional struggles related to the surgery and weight loss.
6. Long-Term Risk of Weight Regain
- While most people successfully maintain weight loss for several years, some may experience weight regain after the first few years. This can occur if patients don’t adhere to the required diet, exercise, and lifestyle changes.
- It is important for patients to stay vigilant about their habits to maintain their weight loss over time.
7. Possible Complications
- Stomal Stenosis: Narrowing of the small opening between the stomach pouch and the small intestine can occur, leading to difficulty eating or vomiting. This may require dilation or further surgery.
- Gallstones: ** weight loss can increase the risk of developing gallstones, which may require treatment or removal of the gallbladder.
- Hernias: Some individuals may develop hernias around the surgical site, which could require surgical correction.
8. ** Mobility and Physical Health
- As weight is lost, many individuals find it easier to engage in physical activity and experience ** in overall physical health, such as increased energy levels and reduced fatigue.

Diet restrictions following weight loss surgery
Diet Restrictions Following Weight Loss Surgery
After bariatric surgery, such as gastric bypass or sleeve gastrectomy, patients must follow specific dietary restrictions to promote healing, prevent complications, and achieve long-term weight loss success. The dietary guidelines typically evolve over time, starting with liquids and gradually advancing to solid foods. Below are key diet restrictions and guidelines to follow after bariatric surgery:
1. Initial Liquid Diet (First 1-2 Weeks)
- Clear liquids: Immediately following surgery, you’ll start with clear liquids like water, broth, and sugar-free clear beverages (e.g., unsweetened tea, crystal light).
- Full liquids: After a few days, you can progress to full liquids, including protein shakes, low-fat milk, and strained soups. These should be consumed in small sips throughout the day to avoid overloading the new stomach.
- Restriction: Avoid sugary drinks, carbonated beverages, and caffeine during this phase, as they can irritate the stomach and contribute to dehydration or discomfort.
2. Pureed Foods (2-4 Weeks)
- Soft, blended foods: Foods should be pureed to a smooth consistency, similar to baby food. Examples include mashed potatoes, scrambled eggs, low-fat cottage cheese, pureed fruits, and vegetables.
- Protein-rich foods: Focus on lean proteins like pureed chicken, fish, and tofu to promote muscle maintenance and help with satiety.
- Restriction: Avoid foods with high fat, sugar, or fiber (which may be difficult to digest), and skip any foods that are overly processed or have hard-to-chew textures.
3. Soft Foods (4-6 Weeks)
- Soft, easily digestible foods: At this stage, you can start introducing soft foods with a slightly thicker texture, such as soft cooked vegetables, lean ground meats, and low-fat cheeses.
- Focus on protein: Protein is essential for healing and weight loss, so aim for protein-rich foods like lean meats, eggs, fish, and legumes.
- Restriction: Avoid raw fruits, vegetables with skins or seeds, and fibrous foods, as they can be difficult to tolerate and cause blockages or discomfort.
4. Solid Foods (6 Weeks and Beyond)
- Gradual introduction of solid foods: You can begin eating solid foods again, but in small, well-chewed bites. Foods like lean meats, whole grains, and cooked vegetables can be reintroduced slowly.
- Chew thoroughly: Chew food well to prevent discomfort and ensure that your body can properly digest it. Eating slowly and taking smaller portions is key to preventing overeating.
- Restriction: Avoid high-fat, greasy foods, and foods that are high in sugar or ** carbohydrates, as they can contribute to weight regain and may cause discomfort (e.g., dumping syndrome, bloating, nausea).
5. Long-Term Dietary Restrictions
- Limit sugary and high-fat foods: Consuming sugary or fatty foods can cause dumping syndrome (nausea, diarrhea, and dizziness). Over time, these foods can also hinder weight loss and affect your long-term health.
- Avoid drinking with meals: Drinking liquids with meals can cause discomfort and make it harder to eat enough solid food. Wait at least 30 minutes after eating before drinking liquids.
- Alcohol: Alcohol can have a stronger effect after bariatric surgery because the stomach’s capacity is reduced. It is generally recommended to avoid alcohol for at least the first six months and consume it cautiously after that. It can also contribute to dehydration and may irritate the stomach.
6. Supplements
- Vitamin and mineral supplements: After bariatric surgery, you will likely need to take vitamin and mineral supplements to avoid nutritional deficiencies. Common supplements include:
- Multivitamins
- Calcium (with vitamin D)
- Vitamin B12
- Iron (especially for women)
- Vitamin D
- Follow-up with a healthcare provider: Regular check-ups and blood tests will help monitor for any deficiencies and adjust supplements accordingly.
7. Hydration
- Drink plenty of water: Staying hydrated is crucial after bariatric surgery. Drink at least 64 ounces of water daily (but not with meals). Sip fluids slowly throughout the day, and avoid caffeinated or sugary drinks, which can dehydrate you and irritate the stomach.

Tips for success after bariatric surgery
Key Tips for Success After Bariatric Surgery:
- To digest food effectively, take small bites and chew food thoroughly to prevent discomfort or blockage.
- Focus on protein: Protein is vital for maintaining muscle mass and supporting healing. Aim to get adequate protein with every meal.
- Small, frequent meals: Instead of large meals, eat smaller portions throughout the day (usually 3 meals and 2-3 snacks).
- Avoid high-calorie snacks: Even healthy foods can contribute to weight regain if consumed in excess, so always stick to portion control.

Bariatric surgery indications and eligibility
Indications/Eligibility
- BMI>30
- Ideal for people who haven’t had long-term success with weight loss through diet and exercise.
Frequency
- Period of Treatment: Once (unless complications or weight regain)
- Mechanisms of Action:
- Restricts eating capacity
- Induces satiety by removing or excluding that part of the stomach that produces hunger hormones
- Increases the production of hunger inducing hormones
- Promotes reduction in absorption of nutrients
- Various neurohormonal interplay brings about reduction in gut contraction and there-by, furthermore, inducing satiety and reducing digestion
Availability
- Mostly in private sector; Should ideally be performed by specifically trained Upper GI surgeon
TBWL: Total Body Weight Loss %
- Sleeve: 20-30%
- Bypass: 25-40%
TBW % Loss Long Term
- Unknown
Potential Risks/Side Effects
- Infection, blood clots, complications from anesthesia., nutritional deficiencies
Serious side effects/ complications
- 1.5 – 4% (Australian Bariatric Registry)
- Leaks, blockages, or long-term digestive issues.
Effects of metabolic syndrome (Diabetes, high cholesterol and related diseases)
- 70% had complete resolution from diabetes after 1 year
- 80% did not need any insulin after 1 year
Recurrence of metabolic syndrome
- 30-50% still remained free from diabetes even after weight gain (suggesting strong neurohormonal effects that last long term) even at 10 years after the operation
Cost
- One time cost
Pros and Cons of Weight Loss Surgery
Pros:
- Significant weight loss: Can result in a substantial reduction in weight, which can ** or resolve obesity-related health issues like type 2 diabetes, high blood pressure, and sleep apnea.
- Long-term results: With proper lifestyle changes, bariatric surgery can lead to sustained weight loss over the long term.
- ** in overall health: People often experience significant health **, including better blood sugar control, lower cholesterol, and reduced risk of cardiovascular disease.
Cons:
- Invasive procedure: Requires surgery, which carries risks like infection, complications, or blood clots.
- Long recovery time: Recovery time can be significant, and the individual may need to modify their diet and exercise routine post-surgery.
- Lifestyle changes required: After surgery, patients need to commit to a lifetime of changes, including a strict diet, regular physical activity, and sometimes vitamin supplementation.
- Irreversible: Most weight loss surgeries, such as gastric bypass, are permanent and irreversible.

How painful is weight loss surgery?
How Painful is Weight Loss Surgery?
The level of pain experienced after weight loss surgery can vary depending on the individual, the type of surgery, and how well they manage recovery. In general, most people report some discomfort and pain after the procedure, but the intensity and duration of the pain are usually manageable with proper care and medication. Here’s a breakdown of what to expect in terms of pain for common weight loss surgeries:
- Pain Level: Right after surgery, you can expect some level of pain or discomfort, typically moderate to mild. This pain is most commonly due to the surgical incisions, gas used during the procedure, and the manipulation of the stomach and intestines.
- Common Areas of Discomfort: The incision sites, bloating or gas pain in the abdomen, and soreness around the chest (from the surgery and the breathing tube used during anesthesia).
- Pain Management: Pain is usually managed with prescription pain medications for the first few days, and many patients are switched to over-the-counter pain relievers (such as acetaminophen) within a week or two.
- Recovery: Pain from the incisions and bloating tends to subside within a few days, but some mild discomfort may persist for up to 2 weeks. Again, pain is generally controlled with prescribed medications initially, transitioning to over-the-counter pain relievers after a short period.
- Long-Term Pain: For most patients, pain significantly diminishes within the first few weeks after surgery. However, some people may experience mild discomfort for longer periods, especially if complications arise, like hernias or an issue with the surgical site.

Choosing the weight loss right surgery
Choosing the right Weight Loss Surgery
Consulting with a bariatric surgeon is essential to determine which option fits your needs, health status, and goals, with each type of weight loss surgery having its own set of advantages and drawbacks. The best choice depends on several factors.
- Gastric Bypass (Roux-en-Y): Reduces the size of the stomach and reroutes the small intestine, limiting food intake and absorption.
- Sleeve Gastrectomy: Removes a large portion of the stomach, leaving a smaller sleeve that restricts food intake.
- Gastric Banding (Lap-Band): Involves placing a band around the stomach to create a small pouch that limits food intake (less commonly performed now).
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): Combines a sleeve gastrectomy with a bypass of most of the small intestine.
Weight loss medications vs weight loss surgery
Key Differences:
- Invasiveness: Medications are non-invasive, while surgery requires a major procedure and recovery time.
- Effectiveness: Bariatric surgery tends to lead to more dramatic and long-term weight loss compared to medications, but both require a commitment to healthy lifestyle changes for the best outcomes.
- Risks: Surgery carries risks associated with the procedure itself, while medications can have side effects but don’t carry the same immediate risks as surgery.
- Suitability: Medications are often used for people with a lower BMI or those who don’t want surgery, while surgery is typically reserved for individuals with severe obesity and related health issues.
- Diet: While a special diet is not mandatory with medications, following a **, balanced eating plan rich in whole foods, lean proteins, and healthy fats while avoiding processed and sugary foods will optimize the results of weight loss injections.
After bariatric surgery, however, patients need to follow a strict diet to allow the stomach to heal and to ensure healthy weight loss. The diet progresses from liquids to pureed foods to solid foods over several weeks. A long-term healthy eating plan, with a focus on protein and avoiding high-sugar or high-fat foods, is crucial to maintaining weight loss.

Weight loss
Final Thoughts
In conclusion, both weight loss medications and surgery offer distinct advantages and challenges, and the choice between the two depends on individual circumstances. Medications may provide a less invasive option with fewer risks, but they typically require long-term commitment and may not lead to as significant weight loss as surgery.
On the other hand, weight loss surgery can result in more dramatic and sustained weight loss, but it involves greater risks, a lengthy recovery process, and significant lifestyle changes. Ultimately, the best approach should be based on a comprehensive evaluation of one’s health, goals, and personal preferences, ideally in consultation with a healthcare professional.
Dr Manjunath Siddaiah-Subramanya

Dr Manjunath Siddaiah-Subramanya
FRACS, MMIS, MSurgEd, FAANZGOSA, Consultant Upper GI Surgeon SWSLHD |, Senior Conjoint Lecturer WSU and UNSW | Director Precision Upper GI Surgery
One of Australia’s leading Upper Gastrointestinal Specialist Surgeons, Dr. Manjunath Siddaiah-Subramanya (Manju) offers a wide range of comprehensive treatment options for those seeking upper gastrointestinal surgical weight loss solutions.
Understanding that each patient’s journey to weight loss is unique, Dr. Manju offers personalised consultations to determine the most effective surgical approach, including procedures such as gastric bypass, sleeve gastrectomy, and revisional surgeries for reflux and weight regain following bariatric surgery.

Weight loss
FAQs
Who is a candidate for gastric bypass surgery?
Candidates for gastric bypass typically have a body mass index (BMI) of 40 or higher, or a BMI of 35 with obesity-related health conditions such as type 2 diabetes, sleep apnea, or heart disease. It is generally recommended for individuals who have been unable to lose weight through diet and exercise alone.
How long is the recovery after gastric bypass surgery?
Recovery time varies by individual, but most patients spend 2-3 days in the hospital after surgery. Most people can return to normal activities within 4-6 weeks, though strenuous physical activity should be avoided for several months. Full recovery may take several months, depending on the person.
What are the risks and complications of gastric bypass surgery?
While gastric bypass is generally **, there are risks, including infection, bleeding, blood clots, nutritional deficiencies, ulcers, and leakage at the site of the surgery. Long-term complications can include gallstones, dumping syndrome (nausea and diarrhea after eating sugary foods), and vitamin and mineral deficiencies.
How much weight can I expect to lose with weight loss injections?
The amount of weight loss varies depending on factors such as the specific medication, dosage, diet, exercise, and individual metabolism. In clinical trials, people using semaglutide (Wegovy) for weight loss have lost an average of 15-20% of their body weight over a year. However, individual results can vary.
Are weight loss injections **?
Weight loss injections are generally considered ** for most people when used under the supervision of a healthcare provider. However, like any medication, they can have side effects. Common side effects include nausea, diarrhea, and constipation. Rare but serious side effects can include pancreatitis, gallbladder issues, and kidney problems. It’s essential to consult a healthcare provider to determine if weight loss injections are appropriate for your health condition.
How long do I need to use weight loss injections?
Weight loss injections are typically used long-term to maintain weight loss. The exact duration of use depends on the individual and their weight loss goals. Once you’ve reached your target weight, your healthcare provider may gradually reduce the dosage, but continuing a healthy diet and exercise regimen is crucial to maintaining results. Stopping the injections too soon may lead to weight regain. Always follow your doctor’s recommendations for continued use and monitoring.