
Obesity is the excessive accumulation of body fat that impacts health. This article examines its causes, consequences, and effective solutions, with a focus on Australia and New South Wales.
The increasing obesity rate in New South Wales, which affects 57.8% of adults, is a significant public health concern. Addressing this requires a comprehensive strategy that includes lifestyle changes, medical assistance, and community programs promoting ** living. Weight loss surgery can be an effective option for many patients.
Understanding Obesity
Obesity is a chronic complex disease marked by abnormal or excessive fat accumulation, which presents a risk to health. It’s more than just carrying extra weight—it involves a complex interplay of genetic, environmental, and behavioral factors that, if not addressed promptly, can lead to numerous health complications. The body mass index (BMI) is a common tool used to diagnose obesity, providing a simple means to categorize individuals based on their weight relative to their height.
Globally, more people are now obese than underweight, except in the South-East Asia Region. This shift marks a significant public health challenge, highlighting the rise of the obesity epidemic. Obesity/ overweight is acknowledged by the World Health Organization (WHO) as part of the ‘double burden of malnutrition,’ a phenomenon where undernutrition and obesity coexist within the same communities and even households. This paradox underscores the complexity of addressing obesity in a world where both excess and scarcity of resources exist.

Appreciating the implications of obesity requires acknowledging its influence on diverse health aspects, spanning from physical to psychological well-being. Excess body fat can lead to numerous health complications, including heart disease, diabetes, and certain cancers. As we delve deeper into this topic, it becomes clear that ** obesity requires a multifaceted approach, tackling its root causes and promoting sustainable solutions.
How Common Is Obesity?
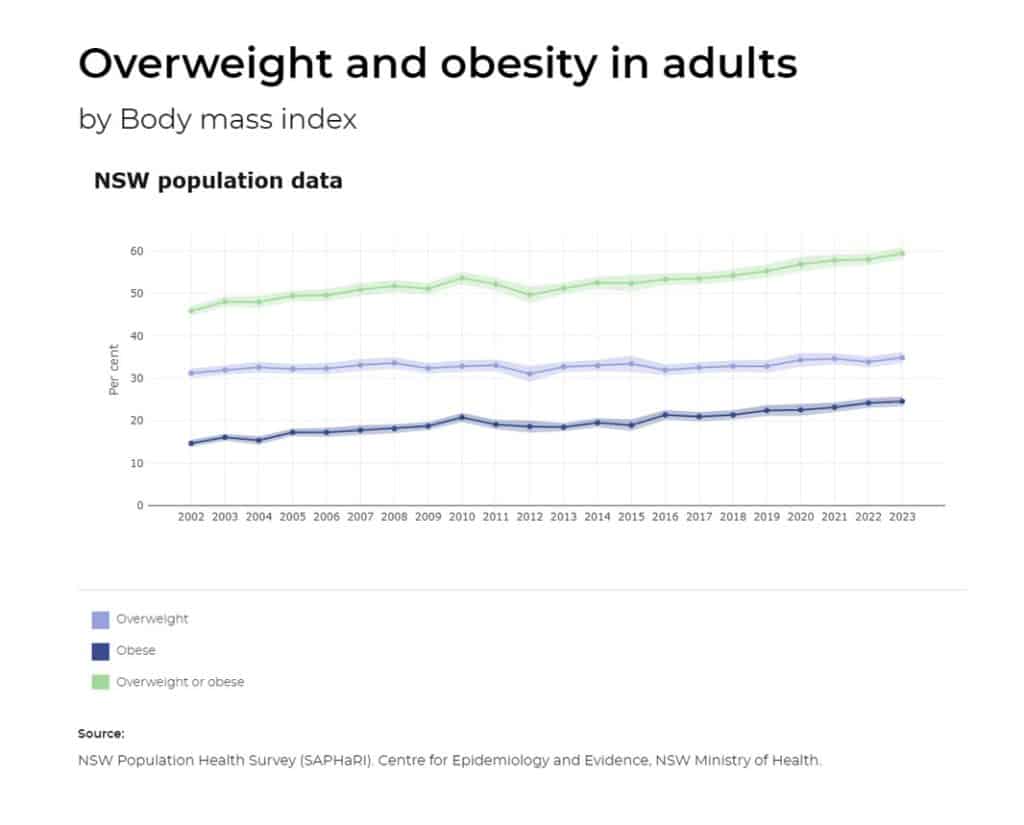
Over the past few decades, the occurrence of obesity has risen dramatically. From 1990 to 2022, the percentage of adults aged 18 years and older living with obesity more than doubled from 7% to 16%. Despite this alarming rise, current monitoring shows a stable trend in the prevalence of obesity since 2017–18. This stability, however, does not diminish the urgency of ** obesity, as the numbers remain significantly high.
The statistics from New South Wales (NSW) present a worrisome scenario. In 2023, 57.8% of adults aged 16 and over were overweight or obese. The prevalence varies significantly across different demographics. For instance, 65% of men and 54% of women aged 16 years and over were dealing with overweight or obesity. These disparities underscore the necessity for targeted interventions that take into account gender-specific factors in managing obesity.
Socioeconomic status significantly influences the prevalence of obesity. In 2023, 69% of people living in the most disadvantaged areas were dealing with overweight or obesity, compared to 51% in the least disadvantaged areas. Additionally, regional disparities exist, with higher obesity rates in inner regional and outer regional or remote areas compared to major cities. These figures emphasize the need to tackle social determinants of health for an effective fight against obesity.
Join Our Free Weight Tracker Today!
Easily track your weight and measurements, and visualize your progress with charts and photos. Sign up for personalized support from our expert team! Start your journey now!
Obesity rates in Maitland, NSW Australia
Maitland, a city in New South Wales, stands out with higher obesity rates compared to the rest of the state. In Maitland, 44.7% of the population is obese, significantly higher than the 30.9% observed statewide. This discrepancy highlights the need for localized public health initiatives tailored to the specific challenges faced by Maitland residents.
A variety of factors contribute to the high obesity rates in Maitland, including socioeconomic conditions and lifestyle choices. Addressing these issues requires a concerted effort from community leaders, healthcare providers, and policymakers to implement effective obesity management and prevention strategies. By focusing on the unique needs of Maitland, it is possible to make significant strides in reducing obesity rates and ** overall public health.
Obesity rates in the Hunter New England and Central Coast Primary Health Network
The Hunter New England and Central Coast Primary Health Network also faces a significant challenge with high obesity rates. This region, which includes local government areas such as Armidale Regional and Central Coast, has a prevalence of overweight and obesity that is a major public health concern. The rates in this health network are among the highest in NSW, underscoring the need for targeted interventions.
Combatting obesity in this region necessitates an inclusive strategy that encompasses community-based initiatives, ** healthcare accessibility, and policies endorsing healthier lifestyles. By understanding the specific factors contributing to obesity in the Hunter New England and Central Coast Primary Health Network, stakeholders can develop more effective strategies to combat this public health issue.
Causes of Obesity
Obesity is a multifactorial disease, stemming from an interplay of genetic, environmental, and psychological factors. Comprehending these causes is vital for devising effective prevention and treatment strategies.
This section will delve into the specific contributors to obesity, including genetic predispositions, environmental influences, and psychological and behavioral factors.

Genetic Factors
An individual’s predisposition to obesity is significantly influenced by genetic factors. Researchers have identified at least 15 genes that influence obesity, making some people more prone to gaining weight and body fat. Polygenic obesity, the most common form, involves multiple genes contributing to a higher risk of weight gain. These genetic predispositions can make it more challenging for some individuals to maintain a healthy weight despite their best efforts.
Monogenic obesity, although less common, results from single-gene mutations and is characterized by severe obesity without developmental delays. Conditions such as Prader-Willi syndrome, a genetic disorder leading to an abnormally increased appetite due to central nervous system dysfunction, further illustrate the complex relationship between genetics and obesity. Understanding these genetic factors is crucial for developing personalized treatment plans for individuals struggling with obesity.
Environmental Influences
Environmental factors also significantly contribute to the obesity epidemic. Some of these factors include:
- Easy access to high-calorie, nutrient-poor foods in many communities
- Neighborhoods with more fast-food restaurants and fewer green spaces
- Sedentary lifestyles encouraged by the environment
These environmental influences create an obesogenic environment that encourages excessive food intake and sedentary lifestyles.
Urbanization and the automation of tasks have led to reduced physical activity, further exacerbating the obesity problem. Additionally, inadequate prenatal, infant, and young child nutrition contribute to the sharp increases in childhood obesity in low- and middle-income countries. Addressing these environmental factors requires systemic changes, including urban planning that promotes physical activity and policies that ensure access to healthy foods.
Psychological and Behavioral Factors
The development of obesity is also heavily influenced by psychological and behavioral factors. Some of these factors include:
- High levels of stress, which can alter hormone levels, increasing hunger and leading to weight gain
- Stress-induced changes in eating behaviors, such as overeating, which are common among individuals struggling with obesity
- Emotional eating, where food is used as a source of comfort during periods of emotional distress, which further contributes to excessive weight gain.
Mental health issues, such as depression and low self-esteem, are more prevalent in individuals with obesity. Some individuals may turn to food for emotional comfort, leading to weight gain as a result of depression. This coping mechanism can contribute to shifts in weight for those struggling with this condition. These factors highlight the importance of ** mental health as part of comprehensive obesity management strategies.
Health Risks Associated with Obesity
Obesity brings with it a host of health risks that can considerably affect an individual’s quality of life. Some of the most concerning risks include:
- Increased likelihood of developing cardiovascular diseases, including heart disease and stroke, due to high blood pressure
- Elevated risk of type 2 diabetes, largely due to associated conditions like hypertension and kidney disease
- Chronic conditions that can lead to severe health complications and even premature death
Cancer is another significant risk associated with obesity. Individuals with obesity are at a higher risk of developing various cancers, including:
- Colon cancer
- Rectum cancer
- Prostate cancer in men
- Breast cancer
- Uterine cancer
- Gallbladder cancer in women
The link between excess body fat and cancer underscores the importance of maintaining a healthy weight to reduce cancer risks.
Some health risks associated with obesity include:
- Breathing problems, such as sleep apnea and asthma
- Increased risk of osteoarthritis due to pressure on joints
- Pregnancy complications, such as gestational diabetes and preeclampsia
These health risks highlight the need for effective obesity management to address risk factors and ** overall health outcomes.
Measuring Obesity
The diagnosis and management of obesity critically depend on its accurate measurement. The primary methods include calculating the body mass index (BMI) and measuring waist circumference. These tools help healthcare professionals assess an individual’s health risks related to excess body fat.
Body Mass Index (BMI)
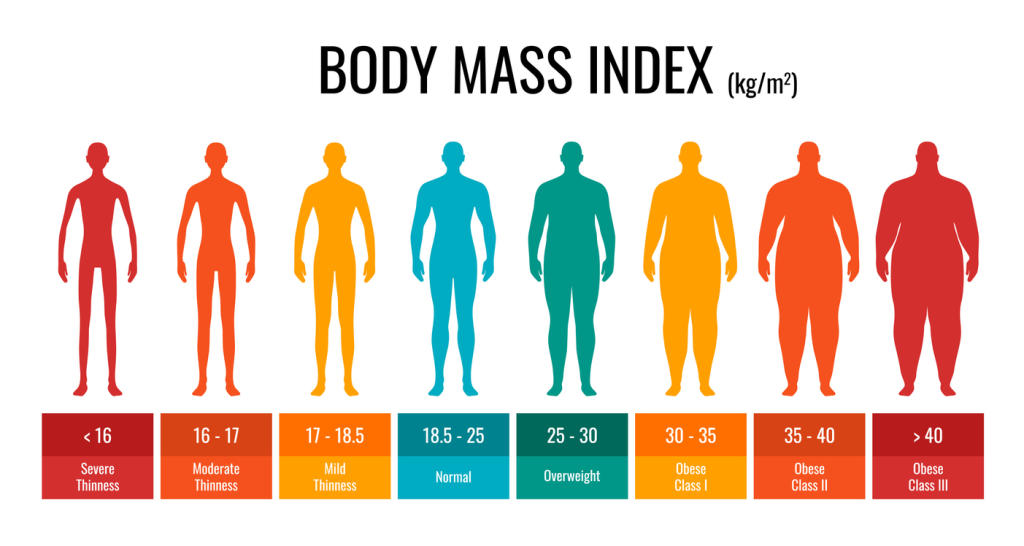
The body mass index (BMI) is a widely used tool for categorizing individuals based on their weight relative to their height. It provides a ** and reliable way to determine if a person’s weight is **. A BMI of 18.5 to 24.9 is considered **, 25 to 29.9 is overweight, and over 30 is classified as obese. However, BMI has its limitations as it does not distinguish between fat mass and muscle mass, nor does it indicate fat distribution. This can make it less accurate for individuals with high muscle mass.
For children, BMI is used differently. In those over two years old, a BMI at or above the 95th percentile for age and sex is considered indicative of obesity. Despite its limitations, BMI remains a valuable tool for initial obesity assessment and monitoring.
Waist Circumference
Waist circumference is another important measure in assessing obesity-related health risks. This method involves measuring the girth around the abdomen, helping to assess fat distribution, particularly visceral fat, which is stored around internal organs and linked to various health issues.
Waist circumference is particularly beneficial for individuals who are muscular, as BMI can be misleading for them. A waist circumference of 94cm or more in men and 80cm or more in women significantly increases the risk of obesity-related health problems. This measure provides a more comprehensive understanding of an individual’s health risks related to body fat.
Managing and Treating Obesity
A blend of lifestyle modifications, medical interventions, and surgical options are involved in managing and treating obesity. These approaches aim to reduce excess body fat and ** overall health outcomes.
Why is it so difficult to loose weight?
The body’s complex biological responses often make weight loss a challenging endeavor. Most overweight individuals face a physiological battle against weight loss, as their bodies try to prevent permanent weight loss. The hypothalamus plays a crucial role in regulating body weight through hormones and neurons that influence appetite and food intake.
When individuals attempt to lose weight, their bodies respond by decreasing leptin, a hormone that signals fullness, and increasing ghrelin, a hormone that stimulates hunger. This hormonal imbalance makes it difficult to maintain weight loss. Additionally, drastic calorie reduction can lead to muscle loss, which is essential for metabolism, and increase the likelihood of rebound overeating. These factors highlight the need for sustainable weight loss strategies that consider the body’s biological responses.
Lifestyle Changes
Obesity management fundamentally relies on lifestyle modifications. Adopting a healthy diet and increasing physical activity are essential steps in achieving and maintaining a healthy weight, as well as avoiding the need to gain weight. Here are some tips for weight management:
- Increase consumption of whole grains, fruits, and vegetables.
- Serve at least five servings of fruits and vegetables daily to ensure a nutrient-rich diet.
- Drink water instead of sugary beverages.
- Avoid using food as a reward or punishment for children to foster healthier eating habits.
Regular physical activity is equally important. At least 150 minutes of moderate-intensity aerobic exercise per week is often recommended for adults, while children should aim for 60 minutes of moderate physical activity most days of the week. Combining aerobic exercise with a balanced diet can lead to a loss of fat mass, even if not necessarily weight. Safe weight-loss programs typically include multiple counseling sessions to support individuals in making lasting lifestyle changes.
Medical Interventions
When lifestyle modifications prove insufficient, the need for medical interventions may arise. Weight loss medications are often prescribed for adults with a BMI of 30 or more, or a BMI of 27 or greater with obesity-related health conditions. These medications, which include appetite suppressants, are typically used in conjunction with diet, exercise, and behavioral therapy to enhance their effectiveness.
While weight-loss medications can help maintain weight loss, they come with potential side effects such as oily and frequent bowel movements, bowel urgency, and an increased risk of thyroid cancer for some medications. Therefore, these medications are usually recommended under careful medical supervision to ensure they are suitable for the patient’s overall health profile.
Surgical Options
Bariatric surgery, or weight-loss surgery, may be a viable option for individuals with severe obesity who haven’t found success with nonsurgical weight loss methods. These surgeries modify the digestive system to help patients lose weight by limiting food intake or reducing nutrient absorption. Doctors may suggest weight-loss surgery for individuals with a BMI of 35 or higher, particularly if they have obesity-related health conditions.
Various surgical options are available, including less invasive endoscopic procedures that are emerging as alternatives to traditional bariatric surgery for certain patients. The recommended age range for individuals with class 1 obesity to undergo surgery is between 18 and 65 years.
Bariatric surgery can be a life-changing intervention, but it requires a commitment to long-term lifestyle changes and medical follow-up to ensure its success.
The Role of Society and Policy in Addressing Obesity
Tackling obesity goes beyond individual efforts, demanding changes at the societal and policy levels. The National Preventive Health Strategy 2021–2030 and the National Obesity Strategy 2022–2032 aim to:
- Prevent, reduce, and treat overweight or obesity in Australia
- Emphasize a whole-of-government approach
- Focus on wider health determinants and reducing health inequities
- Recognize that the root causes of overweight and obesity are complex and embedded in societal systems
- Require systemic changes
Economic policies can significantly influence obesity through various measures taken at community, state, and federal levels, including:
- Promoting healthier food choices
- Increasing access to physical activity opportunities
- Implementing educational programs to raise awareness about the health risks associated with obesity
These initiatives are designed to create an environment that supports healthy living and reduces the prevalence of obesity.
The collaboration between government bodies, healthcare providers, and the food industry is essential to effect meaningful change. By aligning efforts across sectors, it is possible to:
- ** the multifaceted nature of obesity
- Implement effective prevention and treatment strategies
- Create a ** society
- Mitigate the long-term health impacts of obesity
This comprehensive approach is vital for creating a ** society and mitigating the long-term health impacts of obesity.

Obesity in Specific Populations
The occurrence of obesity significantly varies across different population groups, underscoring the need for bespoke interventions. Children and adolescents are particularly vulnerable, with the prevalence of overweight and obesity increasing with age. In 2021, 23.0% of children aged 5-16 in NSW were overweight or obese. Factors contributing to childhood obesity include:
- ** weight gain during infancy
- poor sleep
- having overweight or obese parents
- exposure to marketing of unhealthy foods
** childhood obesity requires early interventions and supportive environments that promote healthy habits.
Aboriginal and Torres Strait Islander populations face higher rates of obesity compared to non-Indigenous populations. In 2018-19, the prevalence of overweight or obesity among Aboriginal and Torres Strait Islander children and adolescents was 38%. Socioeconomic factors, limited access to healthcare, and cultural influences contribute to these disparities. Tailored programs that respect cultural contexts and ** specific needs are essential for effective obesity management in these communities.
Adults living in disadvantaged areas or remote regions also experience higher obesity rates. In 2023, the percentage of people living in the most disadvantaged areas dealing with overweight or obesity was 69%, compared to 51% in the least disadvantaged areas. These disparities underscore the importance of ** social determinants of health and ensuring equitable access to obesity prevention and treatment resources. By focusing on specific populations, it is possible to implement more effective and inclusive obesity management strategies.
Prevention Strategies
Obesity prevention demands a holistic approach, incorporating the promotion of healthy environments and the adoption of preventive interventions throughout the life cycle. Access to sidewalks and green spaces can encourage physical activity and help prevent obesity. Creating supportive environments that promote active lifestyles and healthy eating is crucial for reducing obesity rates.
One of the targets of the National Obesity Strategy is to halt the rise and reverse the trend in adult obesity prevalence by 2030. This ambitious goal requires coordinated efforts across various sectors, including healthcare, education, and urban planning. Another target is to reduce overweight or obesity in children and adolescents by at least 5% by 2030. Early interventions, such as promoting healthy eating habits and physical activity from a young age, are essential for achieving this target.
Changing family eating habits and activity levels gradually can have a significant impact on preventing obesity. Parents who eat healthy foods and engage in physical activity set a positive example for their children, fostering lifelong healthy habits. Adopting preventive interventions at each step of the life cycle, including pre-conception and early years, can help reduce the risk of developing obesity and its associated health complications.
Summary
** obesity in Australia, particularly in New South Wales, requires a multifaceted approach that considers genetic, environmental, and psychological factors. By understanding the complex nature of obesity and its causes, we can develop more effective strategies for prevention and treatment. The health risks associated with obesity, including heart disease, diabetes, and certain cancers, underscore the urgency of tackling this issue.
Measuring obesity through tools like BMI and waist circumference helps healthcare professionals assess health risks and develop personalized treatment plans. Managing obesity involves a combination of lifestyle changes, medical interventions, and surgical options, each tailored to the individual’s needs. The challenges of weight loss highlight the importance of sustainable strategies that consider the body’s biological responses.
Societal and policy-level changes are crucial for creating an environment that supports healthy living. By implementing comprehensive prevention strategies and ** the social determinants of health, we can reduce obesity rates and ** overall public health. Together, we can make significant strides in combating obesity and promoting a ** future for all.
Frequently Asked Questions
The main causes of obesity include genetic predispositions, easy access to high-calorie foods, reduced physical activity, and stress-related eating behaviors. It’s important to ** these factors for effective prevention and management.
Obesity is typically measured using body mass index (BMI) and waist circumference to categorize individuals based on their weight relative to their height and to assess fat distribution and related health risks.
Obesity is associated with various health risks such as heart disease, type 2 diabetes, certain cancers, breathing problems, osteoarthritis, and pregnancy complications, underscoring the importance of managing obesity effectively.
Treatment options for obesity include lifestyle changes such as healthy eating and physical activity, medical interventions like using weight loss medications, and surgical options such as bariatric surgery. These options are designed to reduce body fat and enhance overall health.
Society and policy can address obesity by implementing initiatives such as the National Preventive Health Strategy and the National Obesity Strategy, which aim to create supportive environments, promote healthy food choices, and increase access to physical activity opportunities. These measures can contribute to reducing obesity in the population.